Cannabis is the most widely used illicit drug. Over the last thirty years, the average age of first marijuana usage has fallen and its lifetime prevalence has risen in most developed countries. Cannabis' popularity is derived from the mild euphoria associated with its consumption and from the generally held belief that its health consequences are rather benign. However, there is growing evidence of an association between mental health problems and cannabis use (Degenhardt et al. 2003; Arseneault et al. 2004). What remains unclear is whether the proper interpretation of this evidence is that cannabis use causes mental health problems. The existence of unobserved personal characteristics or circumstances that cause both mental illness and cannabis use is a plausible alternative explanation. In recent work, we use the 2004 Australian National Drug Strategy Household Survey (NDSHS) to examine whether cannabis use leads to worse mental health.
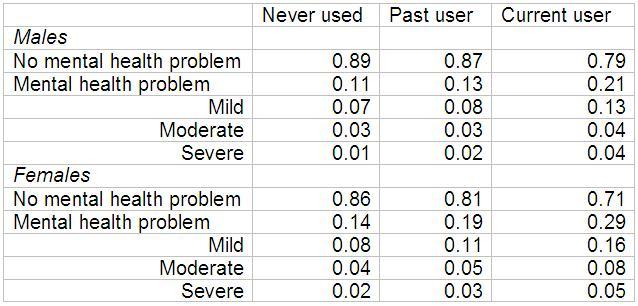
Table 1 presents the relationship between current mental health status and cannabis use is shown for males and females aged 26-50. It shows that mental illness is more common among current and past users of cannabis compared to those who have never used. For example, we see that 11% of males and 14% of females who have never used cannabis have a mental health disorder compared to 21% of males and 29% of females who are current users. Table 1 also shows that past cannabis users are less likely to currently suffer mental illness compared to current cannabis users. For example, 13% of males and 19% of females who are past users of cannabis are classified as having a mental health disorder compared to 21% of males and 29% of females who are current users. The third stylised fact that emerges from Table 1 is that females are more likely than males to suffer mental illness.
Table 1. Mental illness conditional on cannabis use
Note: Mental health status is measured by the Kessler-10 (K10) scale of psychological distress, which is a self-report measure of psychological distress consisting of 10 items which ask respondents about symptoms of depression and anxiety in the past four weeks.
These patterns are not unique to Australia and there is substantial evidence that cannabis use is associated with greater levels of mental illness. But this evidence does not necessarily imply a causal relationship. It may simply reflect a common unobserved factor, such as a genetic characteristic, that makes people vulnerable to both cannabis use and mental illness. Indeed, the most significant challenge faced when investigating potential links between cannabis use and mental health is the impossibility of observing all the personal characteristics and circumstances that might be relevant. According to Pudney (2010), even the most comprehensive longitudinal survey cannot hope to measure every relevant aspect of the individual and his or her environment. Nevertheless, in order to be able to assess the potential causal link between cannabis use and mental health common, we must account for unobserved “confounding" factors that may be a source of spurious association.
Our research uses a discrete factor approach to account for the potential for common unobserved confounders. Our methodology marries Heckman and Singer's (1984) use of discrete factors in addressing unobserved heterogeneity in hazard rate analysis with their use by Mroz (1999) to account for endogenous variables in regression models. More specifically, we estimate a trivariate system of equations consisting of hazard functions for the decision to start using cannabis and the decision to quit and a Tobit model for the production of mental health. By allowing the distribution of discrete factors determining cannabis use dynamics and continuous mental health to be correlated, we account for common unobserved factors and hence obtain reliable estimates of the impact of cannabis use on mental health.
In order to illustrate our findings, we use our estimates to simulate the mental health of different types of cannabis users, ranging from non-users to daily cannabis users. The simulations results are presented in Table 2.
Table 2. Simulated effects of cannabis use on mental health problems
Simulated individual: Australian-born, non-aboriginal, forty year-old educated more than ten years and married.
They show that, for males, the impact of using cannabis weekly or more often produces a substantial increase in the prevalence of mental illness compared to those who have never used, used in the past, and those who use less frequently. The prevalence of mental illness amongst males using cannabis frequently (weekly or more often) is predicted to be 14.3% to 14.8%. In comparison, otherwise similar males who have never used cannabis are predicted to have a prevalence of mental illness of 8.0%. This increase occurs predominantly among the categories of mild and severe mental illness. For example, Table 2 shows that the prevalence of severe mental illness in males who use cannabis weekly (or daily) is double that of males who have never used cannabis (2.4% compared to 0.9%). The simulations also show that less frequent use of cannabis produces a small increase in the prevalence of mental health problems, similar in magnitude to the increase associated with past cannabis use. For example, the prevalence of severe mental distress amongst those who use cannabis once a month is 1.5% compared to 1.4% amongst past users. Intensity of use is found to have a similar effect on females, except that using every few months rather than weekly appears to be the critical use category and females generally experience a higher rate of mental health problems compared to males.
In summary, our results suggest that cannabis use does have an adverse effect on mental health, with frequent current use having a larger effect than infrequent current use or past use. We also find that unobserved factors that make individuals more susceptible to cannabis use also make them more susceptible to mental illness.
While accounting for common unobserved factors reduces the size of the estimated effects of current and past cannabis use on mental health, it does not eliminate them.
References
Arseneault, L., Cannon, M., Witton, J. and Murray, R.M. (2004) “Causal association between cannabis and psychosis: examination of the evidence”. British Journal of Psychiatry 184, 110-117.
Degenhardt, L. Hall, W. and Lynskey, M., 2003. “Exploring the association between cannabis use and depression”. Addiction 98, 1493-1504.
Heckman, J.J. and Singer, B., 1984. “A method for minimizing the impact of distributional assumptions in econometric models for duration data.” Econometrica 52, 271-320.
Mroz T.A., 1999. “Discrete factor approximations in simultaneous equation models: Estimating the impact of a dummy endogenous variable on a continuous outcome.” Journal of Econometrics 92, 233-274.
Pudney, S., 2010. “Drugs policy - what should we do about cannabis?” Economic Policy, forthcoming.
Van Ours, J.C. and Williams, J., 2009. “Cannabis use and mental health problems”, CEPR Discussion Paper, No. 7384