The speed and reach of the COVID-19 contagion is unprecedented in recent history. Originating in Wuhan, China in late December 2019, the SARS-Cov-2 virus has claimed more than 400,000 lives in less than six months. That 90% of the globe recorded infections to this new disease in less than three months leaves little doubt about one of the major culprits: commercial passenger flights make any point on the globe reachable within 48 hours. While air travel brings significant economic and social benefits, it also fosters pathogen transmission. As Mangili and Gendreau (2005) note: “[passenger air travel] can have an important role in the rapid spread of newly emerging infections and could potentially even start pandemics.”
In the absence of viable treatments or vaccines, non-pharmaceutical interventions (NPIs) are century-old recipes to limit the spread of a pathogen (Voth 2020). Restrictions on passenger air travel serve the same purpose as other NPIs such as closing schools, restricting gatherings, canceling public events, and limiting individual mobility: reduce the susceptibility of being infected, isolate those who are, and limit the spatial diffusion of the disease. NPIs certainly contributed to the deceleration of the COVID-19 contagion and prevented a great many deaths (3.1 million in Europe alone, according to Flaxman et al. 2020)
Are passenger air travel restrictions worth implementing in regard to the economic costs they impose? To answer that type of question, economists follow a standard procedure: confront economic losses (measured by GDP) with the monetary value of lives saved by the policy. While estimating the cost of closing air traffic is relatively straightforward, evaluating the benefits is challenging. First, various NPIs have been imposed on a tight schedule, making the identification of individual effects difficult. Therefore, the impact of general lockdowns and overall containment measures have received the lion’s share of economists’ interest (Hargreaves Heap et al. 2020, Santos-Pinto and Mata 2020, Baldwin and Weder di Mauro 2020). Second, the notion of the monetary value of human life is an elusive concept, with estimates varying greatly based (among other factors) on the age of the victims. Any cost-benefit analysis is therefore highly dependent on the chosen ‘value of a statistical life’.
Estimating the influence of passenger air traffic on COVID-19 propagation
Based on an appraisal of the contribution of air travel in the spatial diffusion of COVID-19 across the globe, in this column we present a ‘ballpark’ assessment of the cost-effectiveness associated with passenger air travel restrictions at the height of the epidemic (mid-March to mid-April 2020). In Gonne and Hubert (2020), we show that the conclusions of short-run cost-benefit analysis of air travel restrictions highly depend on a handful of parameter values.
Because the contagion process of COVID-19 is spatial in nature, economists need to use instruments that match the task at hand. In line with this requirement, we rely on spatial econometrics techniques to measure the contribution of commercial air travel to the total number of recorded cases in OECD members and countries hosting the 50 largest airports.
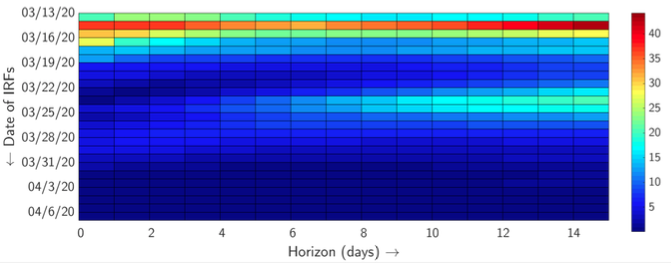
Our model finds that, on average, 8-9% of cases recorded domestically can be attributed to air traffic. Daily observations allow us to have a very precise view of how this influence varied across time. Figure 1 presents the contribution of foreign cases imported through airlines in domestic infections from one to 15 days after being recorded (between 13 March and 22 April 2020). We can distinguish two waves quite clearly: one in mid-March and one in the fourth week of March. April shows a dramatic drop in the influence of foreign cases on local diffusion. By then, most of the flight routes had closed, bringing credence to commercial flights being a sensible vector of pathogen propagation.
Figure 1 Time-varying contribution of foreign cases to domestically recorded Covid-19 cases
Cost-benefit analysis of air travel restrictions
On the cost side, the OECD (2020) evaluates the potential direct economic impact of widespread containment measures based on an output approach. This is done by looking at detailed categories of output, identifying the sectors most directly affected. The OECD’s disaggregated estimates suggest that the output loss in the sector of air transport, accommodation, and food services amounts to about 2.5% of GDP. For our purpose, we disaggregate air transport from the hotel and restaurant activities. In the OECD, air transportation activities typically represent 20% of the latter aggregate. Moreover, the impact on annual GDP growth depends on the duration of the containment measures. In this computation, we consider a four-week extension of air travel restrictions. With an aggregate GDP of $96,000 billion for our panel of 48 countries in 2019, we estimate the cost side of our analysis at $37 billion.
On the benefit side, our model enables us to quantify the death toll associated with being tightly connected by aerial routes. In absolute terms, we estimate that 178,675 cases (and 13,715 deaths) could have been avoided had passenger flights been stopped worldwide on 13 March 2020 for four weeks. Going further, the value attributed to a human life is an elusive concept: how much is the life of an 80-year-old or a 9-year-old worth? How does one account for the ‘loss of a chance at life’? Estimates of this vary significantly. The OECD (2012) suggests that human life be valued at between $1.5 million and $4.5 million, with a base value of $3 million. Viscusi and Masterman (2017) report that a human life is worth $9.6 million. Using the OECD base value, we estimate that stopping all passenger air traffic worldwide in mid-March would have brought a monetary benefit of $44 billion.
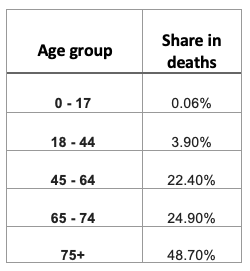
Our ballpark assessment suggests that a global freeze of passenger air transportation could pass a cost-benefit test in the short term. There is, however, considerable uncertainty about that conclusion. In particular, the precise value of life appears to be the factor that tips the scales in favour of (or against) a generalised air passenger transportation shutdown. Instead of using a single value as above, a closer look at the age profile of the deceased shows that COVID-19 disproportionately affect the elderly and people with underlying health conditions. The NYC Health Department reports the share of age groups in the total death toll (see Table 1). Based on standard values of life expectancy at age 65 in OECD countries, we calculate the ‘lost years of life’ for a typical COVID-19 victim as being 15.5 years. The monetary value of a ‘quality-adjusted life year’ (QALY) is also tricky to pin down, ranging from $50,000 to $150,000 per QALY (Neumann et al. 2014). Consequently, a typical casualty from COVID-19 represents a monetary value of between $775,000 and $2.3 million. In addition to this, Hargreaves Heap et al. (2020) and Carrieri et al. (2020) illustrate that framing effects can change people’s valuation of lockdown costs and health benefits. It follows from that conclusion that an analysis on the basis of its perceived costs and benefits may differ from a purely monetary comparison.
Table 1 Age distribution of Covid-19 deaths in New York City
The simulation tool below (accessible by clicking on Figure 2 and hosted here) illustrates how a handful of parameters can change the conclusions above. Moving the sliders affect the number of reported cases, deaths, the monetary value of lives, and, eventually, the cost and benefit sides of the analysis.
Figure 2 Cost-benefit simulation of passenger air transportation during the Covid-19 epidemic
*/
/*-->*/
/*-->*/
Value of a statistical
life (in $1,000):
Share of aviation industry
in GDP (in %):
Share of imported cases
in total cases (in %):
Summary
| (USD bn) |
48 countries |
|---|
| Benefit |
|
| Cost |
|
New cases
(03-13 -- 04-22) |
2364738 |
Deaths
(03-13 -- 04-22) |
176289 |
New cases
due to air travel |
|
Deaths
due to air travel |
|
Duration of
restrictions
(in weeks) |
4 |
//-->
//-->
Source: Based on Gonne and Hubert (2020)
From a policy perspective, it is not our place to conclude on the soundness of the decisions taken at the beginning of the epidemic because we greatly benefit from the advantage of hindsight. Although our calculations can only be characterised as ballpark approximations, we nevertheless regard them as useful points of reference for policymakers – especially at a time when governments discuss re-opening national airspaces and borders. Decisions regarding international travel should also be tailored to the specificities of the country in question. The simulation tool presented here allows for this flexibility.
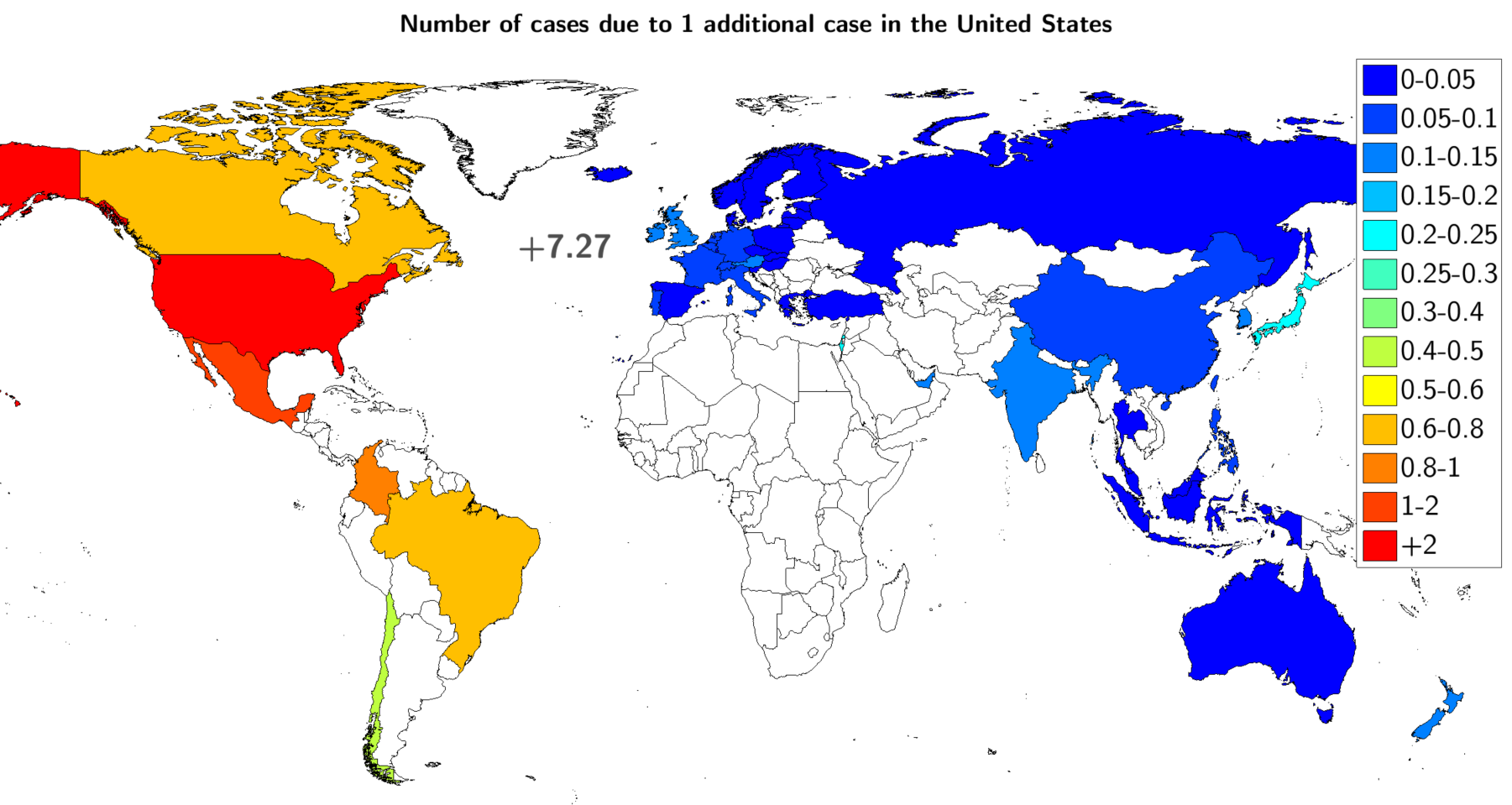
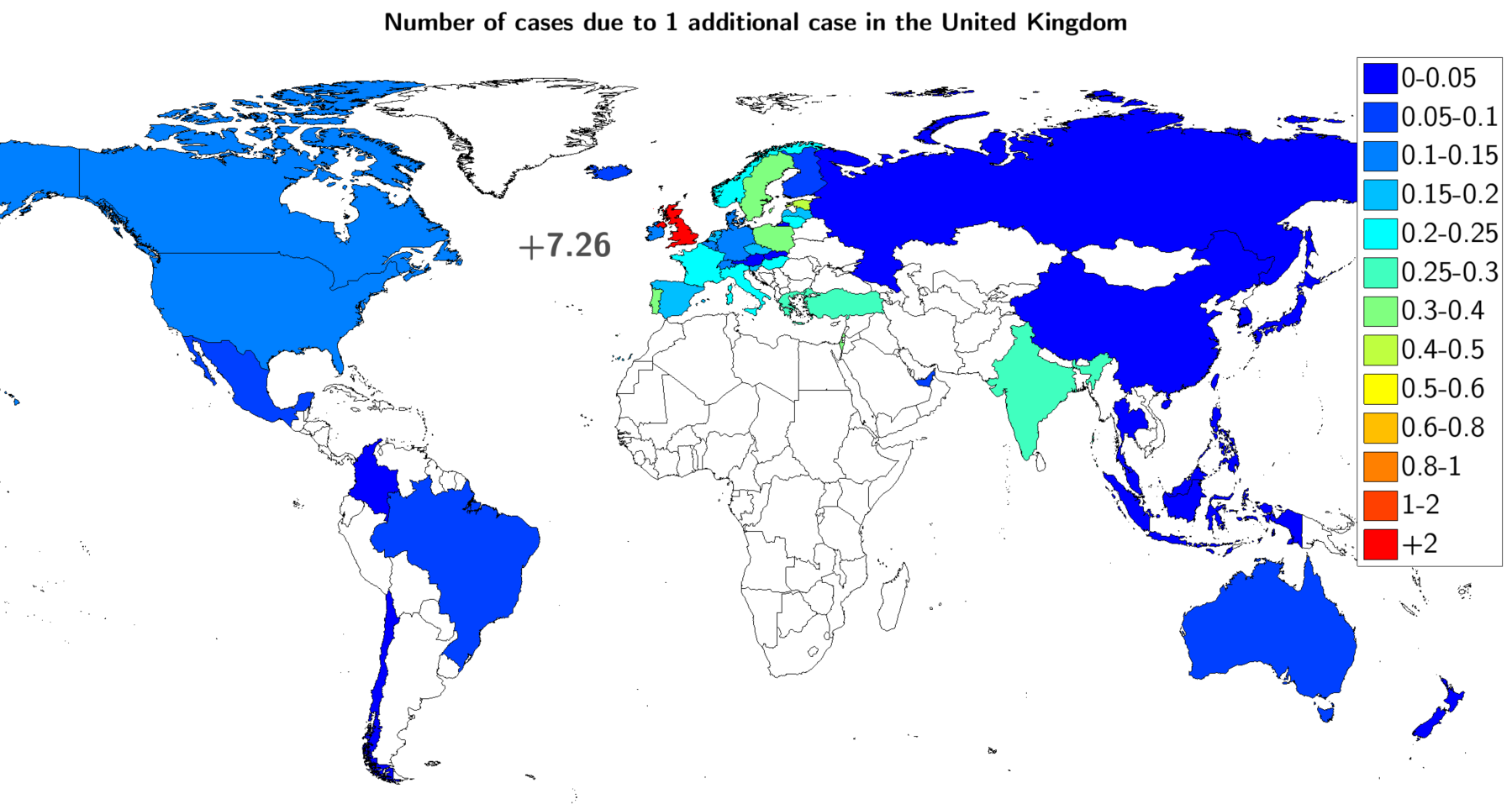
In addition to this, the connectivity structure affects the extent of international contagion, conditioning the usefulness or duration of travel bans as a result. To illustrate the last point, we compare how a newly detected case in the US and the UK spreads to the rest of the world (Figure 3). The US is a ‘super-spreader’ because of the large externalities that additional infections create for the rest of the world, especially in the Americas. The UK example differs from the US because it remains comparatively contained within European countries, Turkey, and India. The decision to re-open the national airspace may require a targeted approach.
Figure 3 Heterogeneous spatial transmission of infections
For all those reasons, a definite conclusion on the cost-effectiveness of air travel restrictions is hard to reach given country-specific features and, most importantly, the difficulty to pinpoint the value of a human life. Blanket restrictions are therefore likely to fail the cost-benefit test. Instead, we advocate a more targeted and coordinated approach. This is essential because a country could enforce a strict lockdown, stop the spread of the virus, and then see its infection rate spike again, warranting a new (hopefully lighter) lockdown, simply because individuals from a highly affected area were allowed to freely travel. The European Commission “Re-open EU” initiative and its real-time dashboard are steps in the right direction.
Authors’ note: The authors are writing in a personal capacity. The views expressed do not necessarily represent the views of the OECD or its Member countries or those of the Banque de France or the Eurosystem.
References
Baldwin, R and B Weder di Mauro (2020), Economics in the Time of COVID-19, VoxEU eBook, CEPR Press.
Carrieri, V, M De Paola and F Gioia (2020), “The impact of communication on people’s preferences for the COVID-19 emergency management”, VoxEU.org, 10 June.
Ferguson, N M, D Laydon, G Nedjati-Gilani et al. (2020), “Impact of non-pharmaceutical interventions (NPIs) to reduce COVID-19 mortality and healthcare demand”, MRC Centre for Global Infectious Disease Analysis, COVID-19 report.
Flaxman, S, S Mishra, A Gandy, H J T Unwin et al. (2020), “Estimating the number of infections and the impact of non-pharmaceutical interventions on covid-19 in 11 European countries”, MRC Centre for Global Infectious Disease Analysis, COVID-19 report 13.
Hargreaves Heap, S P, C Koop, K Matakos, A Unan and N Weber (2020), “Valuating health vs wealth: The effect of information and how this matters for COVID-19 policymaking”, VoxEU.org, 6 June.
Gonne, N and O Hubert, “Spatial distancing: air traffic, COVID-19 propagation, and the cost efficiency of air travel restrictions”, CEPR Covid Economics: Vetted and Real-Time Papers 24: 111-125.
Mangili, A and M Gendreau (2005), “Transmission of infectious diseases during commercial air travel”, The Lancet 265 (9463): 989-996.
Neumann, P J, J T Cohen and M C Weinstein (2014), “Updating cost-effectiveness – The curious resilience of the $50,000-per-QALY threshold”, The New England Journal of Medicine 371: 796-797.
New York City Health (2020), Daily Data Summary, 12 May.
OECD (2012), “Mortality risk valuation in environment, health and transport policies”, Paris: OECD.
OECD (2020), “Evaluating the initial impact of covid-19 containment measures on economic activity”, OECD Policy Responses to Coronavirus (COVID-19).
Santos-Pinto, L and J Mata (2020), “Strategies for Covid-19: The option value of waiting”, VoxEU.org, 22 May.
Viscusi, K W and C J Masterman (2017), “Anchoring biases in international estimates of the value of a statistical life”, Journal of Risk and Uncertainty 54 (2): 103–128.
Voth, J (2020), “Trade and travel in the time of epidemics”, in Baldwin, R and B Weder di Mauro (eds.) Economics in the Time of COVID-19, VoxEU eBook, CEPR Press.