The human potential lost due to poor health is immense, in particular in low-income and middle-income countries. In 2012, as much as 74% of potential healthy life years were lost in Africa, two-thirds of which were due to communicable diseases (Murray et al. 2015). In an international effort to reduce this health burden, the UN is spearheading the drive to end the epidemics of communicable diseases and to provide universal access to basic healthcare through the Sustainable Development Goals. Development assistance for health is an important instrument in attaining these objectives, and has more than quintupled since 1990 to reach $36 billion per year in 2014 (measured in 2014 dollars) (Dieleman et al. 2015).
In order to improve global health outcomes, an important, but controversial, question is how development assistance for health should be allocated across countries and over time. The nine largest multilateral organisations rely heavily on the present level of gross national income (GNI) per capita in their eligibility criteria and allocation formulas.1 Indeed, several articles have suggested that higher levels of national income are associated with better health outcomes (Preston 1975, Pritchett and Summers 1996), although this relationship has been contested by others (e.g. Deaton 2013).
In a recent paper, we analyse the determinants of health outcomes using cross-country data for 99 countries in 2012 (Sterck et al. 2018). Instead of GNI per capita, we find that a country’s epidemiological surroundings, poverty gap, and institutional capacity are significant predictors of health outcomes. Our paper therefore questions major donors’ paradigm of placing a strong emphasis on GNI per capita in their allocation decisions. Moreover, we contribute to the literature on health outcomes and universal healthcare coverage by deriving a healthcare poverty line of 10.89 international dollars per day as an indication of the level of income that an individual needs in order to finance basic healthcare when free, universal healthcare coverage is lacking. Furthermore, we propose a way of measuring the epidemiological surroundings of countries, which we show to be the most important factor affecting health outcomes. Our paper is part of a broader special issue on innovative methods for global health aid allocation that suggests moving beyond GNI in the allocation of aid (Bump 2018).
Determinants of health outcomes
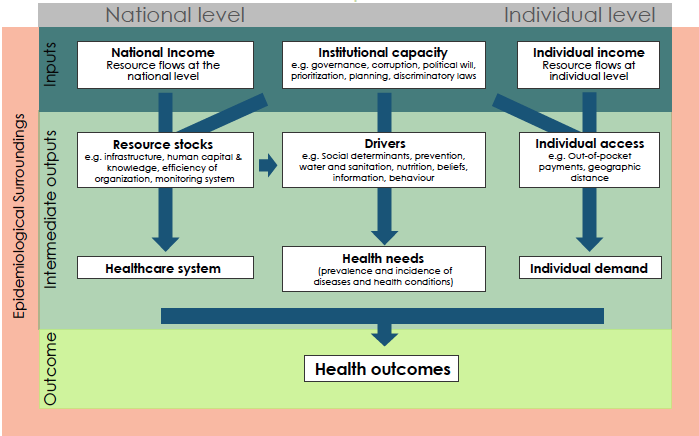
Figure 1 shows the health value chain, which is a simplified representation of the determinants of health outcomes. National income is a primary input for the domestic capacity to invest in health. As a second input, the institutional capacity is fundamental for the construction of an efficient and accessible health system. Financial resources at the individual level affect whether individuals have sufficient income to purchase basic healthcare; these are thus a third input. The national health value chain is embedded in the country’s epidemiological surroundings, which we operationalise as the average disease burden in a country’s neighbouring countries. Many communicable health problems are transboundary by nature, particularly in poorer areas where outbreaks of infections spread more easily because of poor sanitation and governance (Bonds et al. 2010). These primary inputs affect the quality of the healthcare system, health needs, and individual demand for healthcare, ultimately determining the health outcomes of a country.
Figure 1 The health value chain within the epidemiological surroundings
In line with Figure 1, we empirically assess whether GNI per capita, the institutional capacity, individual financial resources, and the epidemiological surroundings determine healthcare outcomes. We measure health outcomes by the disability-adjusted life years (DALYs) per 100,000 people. One DALY is the equivalent of 1 year in good health lost because of premature mortality or disability (Murray et al. 2015). Three categories of DALYs are distinguished:
- Group I DALYs lost due to communicable, maternal, perinatal, and nutritional conditions;
- DALYs lost due to non-communicable diseases; and
- DALYs lost due to injuries.
We focus on Group I DALYs, which are very high in low- and middle-income countries compared to richer countries, as shown in Figure 2. Moreover, Group I DALYs could be more effectively controlled through a well-functioning health system, which can be seen from the observation that log GNI per capita has a clear association with log Group I DALYs (R² of 0.73; elasticity of -0.88) but much less with log DALYs lost due to non-communicable diseases (R² of 0.48 and elasticity of -0.13).
Figure 2 Scatter plots between GNI per capita and two types of health outcomes for 140 countries
The health poverty line and epidemiological surroundings
To measure the determinants of health outcomes, we first derive the poverty gap below the health poverty line of 10.89 international dollars per day, in order to measure individual financial resources. This poverty line is an indicator of the amount of income an individual needs to purchase basic health services, taking available estimates of the costs of basic healthcare and assuming that individuals spend 5% of their income on health goods and services (Taskforce on Innovative International Financing for Health Systems 2009, McIntryre and Meheus 2014).
We measure the epidemiological surroundings by a weighted average of Group I DALYs in neighbouring countries. To avoid simultaneity bias, we apply a spatial lag two-stage least squares regression model (Drukker et al. 2013). We measure GNI per capita in international dollars, and the institutional capacity using World Bank data.
Results and implications
Our results indicate that log GNI per capita is not a significant predictor of health outcomes once the other determinants are included. The poverty gap below the 10.89 international dollars a day health poverty line is a good measure of universal access to healthcare. It explains 19% of deviations in health outcomes, whilst further tests show that the poverty gap below the 1.90 international dollars a day poverty line used by the World Bank to measure extreme poverty is not a significant predictor. The epidemiological surroundings in which countries are embedded capture as much as 47% of deviations in health outcomes. The significance of the epidemiological surroundings appear to be a consequence of the contagious nature of the diseases of Group I DALYs lost, as the epidemiological surroundings are not significant when focusing on the burden of non-communicable diseases. Finally, institutional capacity explains 10% of deviations in health outcomes. Our results remain robust when we use instruments for GNI per capita and the poverty gap, use variation over time or different indicators of health outcomes and institutional capacity, or when we include other predictors of health outcomes mentioned in the literature.
Our findings are relevant for the debate on the allocation of development assistance for health in order to reach the Sustainable Development Goals. GNI per capita is not a direct determinant of health outcomes, even though it might be a reasonably good proxy for health once other factors are ignored. Moreover, GNI per capita is indicative of countries’ capacities to finance healthcare domestically. The importance of individual poverty in explaining health outcomes suggests that the level of GNI per capita fails to reflect the degree of universal healthcare coverage and the inclusiveness of income in a country (Nolan et al. 2018). GNI per capita also does not fully capture the potentially contagious and transboundary nature of communicable diseases. The significance of institutional capacity as a determinant of health outcomes suggests that the quality of governance matters for building a strong healthcare system.
Our finding suggests that the predominance of relying on average income (GNI per capita) as the key metric in allocating development assistance for health is questionable. Our research suggests several metrics that donors can use as alternatives or that can play a complementary role. In which ways these metrics enter the allocation formulas for development assistance of donors will depend on the development goals and the donor's priorities.
References
Bonds, M, D C Keenan, P Rohani and J Sachs (2010), “Poverty trap formed by the ecology of infectious diseases”, Proceedings of the Royal Society of London Series B Biological Science 277: 1185–92.
Bump, J (2018), “Global health aid allocation in the 21st century”, Health Policy and Planning 33(1): 1-3.
Chi, Y and J Bump (2018), “Resource allocation processes at multilateral organizations working in global health”, Health Policy and Planning 33(1): 4-13.
Deaton, A (2013), The Great Escape: Health, Wealth, and the Origins of Inequality, Princeton: Princeton University Press.
Dieleman, J, C Graves, E Johnson, et al. (2015), “Sources and focus of health development assistance, 1990–2014”, JAMA 313: 2359–68.
Drukker, D, I Prucha and R Raciborski (2013), “Maximum likelihood and generalized spatial two-stage least-squares estimators for a spatial-autoregressive model with spatial-autoregressive disturbances”, The Stata Journal 13: 221–41.
McIntyre, D and F Meheus (2014), “Fiscal space for domestic funding of health and other social services”, Centre on Global Health Security Working Group Papers, Working Group on Financing, Paper 5.
Murray, C J L, R M Barber, K J Foreman, et al. (2015), “Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990–2013: quantifying the epidemiological transition”, Lancet 386: 2145–91.
Nolan, B, M Roser and S Thewisssen (2018) “GDP per capita versus median household income: What gives rise to the divergence over time and how does this vary across OECD countries?” Review of Income and Wealth, forthcoming.
Preston, S H (1975), “The changing relation between mortality and level of economic development”, Population Studies 29: 231–48.
Pritchett, L and L Summers (1996), “Wealthier is healthier”, Journal of Human Resources 31: 841–68.
Sterck, O, M Roser, M Ncube and S Thewissen (2018), “Allocation of development assistance for health: Is the predominance of national income justified?” Health Policy and Planning 33(1): 14-23.
Taskforce on Innovative International Financing for Health Systems (2009), Constraints to scaling up and costs: Working Group 1 Report, Geneva: WHO.
Endnotes
[1] These are the WHO, World Bank, Gavi, UNAIDS, UNICEF, UNDP, UNFPA, UNITAID, and the Global Fund (see Chi and Bump 2018).