Governments around the world are tackling the COVID-19 pandemic from different angles. This reflects uncertainty on some key medical facts, to be expected for any new disease. It also incorporates framing effects (Tversky and Kahneman 1981): the way in which the problem is framed may condition and potentially hurt response efforts, even as new data becomes available. A choice is sometimes presented between business-as-usual options that keep the economy running, at some tolerable cost in terms of public health and accepting a number of unavoidable losses in terms of human lives, and lockdowns that save lives but ‘kill’ GDP. The choice is only apparent, as the first option is very unlikely to be sustainable from a political standpoint – at least in democracies with free information. The real point, however, is that in the absence of coordinated containment measures, the most likely outcome is the worst of both worlds: preventable loss of lives and of GDP. Lack of coordination might also lead to erosion of trust between countries, precipitating a persistent reduction in economic openness far in excess of that implied by short-term coordinated reductions in activity and mobility.
Drawing scenarios from available information
Although new evidence on COVID-19 emerges by the hour, uncertainty around its characteristics still abounds.1 Building on the literature on past epidemics and on data from the very first outbreaks, it is still possible to build scenarios for how the virus might spread. Crucially, outcomes depend on the extent, timing and effectiveness of containment measures implemented by governments.
Possible outcomes should fall between two scenarios. At one extreme, the entire global population goes on lockdown for a certain period of time, starting today. At the other extreme, no containment whatsoever is implemented.
An ideal lockdown allowing to achieve zero in-person social interaction would imply no new infections and the progressive eradication of the virus. Its duration would be limited to a few weeks,2 and if started today it would leave global deaths in the low tens of thousands – a simple projection of current mortality rates on those who are already ill. In a milder, more realistic version of a lockdown, social interactions would not be completely eliminated, but reduced through a mandatory stop of nonessential activities.3 Proportional to the rate of actual social distancing achieved,4 the spread of the virus would slow down, preventing healthcare systems from being overwhelmed. If the initial lockdown did not manage to drive spread down to zero in the short run, intermittent follow-ups may be the most effective solution in suppressing the virus over the medium term, while a cure or a vaccine is found (Ferguson et al. 2020). In any version of a lockdown, GDP losses would of course be significant, if temporary.5
In the no-containment scenario, between 40% and 70% of the global population could be infected (as quoted, for example, in Baldwin and Weder di Mauro 2020). A conservative figure (50%) implies 370 million people infected in Europe6 alone over the whole course of the epidemic. Taking what currently appears a prudent estimate of a true case fatality rate (CFR) of 1%, primary deaths would be around 3.7 million, or near half of total European deaths for any cause in 2018.7 In some countries at least, second-round effects resulting from healthcare congestion (affecting both COVID-19 and other patients) could push the number of fatalities up by a non-trivial factor.8 Deaths would still be concentrated, but not limited to, the older populations. Poorer countries and households would also be disproportionately affected.
These outcomes would be still associated with an important fall in GDP – difficult to quantify but probably less short-lived. There would be a direct effect on labour supply due to deaths and the inability to work of all who are seriously affected, either because they fall ill or because they have sick or recovering family members.9 A drop in consumption propensity would dent aggregate demand. Tears in the social fabric may emerge in the hardest-hit areas or sub-populations, probably more worrying than any short-lived unrest brought on by lockdown fatigue.
Uncertainty, lockdowns, and the case for policy coordination
Real-world policies are likely to fall somewhere in between those two scenarios. Yet, we should not be mistaken in assuming that there is a continuum of combinations among which we can choose – a smooth, if painful, trade-off. Apart from the structure of social preferences, relationships are highly nonlinear. While something a little short of the hypothetical radical lockdown is still likely to work, after a certain threshold of social interaction – which, unfortunately, we do not know – any choices would likely yield the second scenario in terms of human losses, without avoiding the economic costs of the lockdown itself.
One very material risk in this sense is inconsistency and unpredictability in the policy response, both in the spatial and the temporal dimension. Again, let’s take Europe as an example. There is free circulation of individuals in the EU, and frequent travel between EU and non-EU countries. Any individual country could go on lockdown for the necessary time, and stop the spread of the virus within its borders, only to find itself fighting the same battle all over again once the lockdown is lifted and travellers come in from other countries where the number of positive individuals is still high because the infection was allowed to spread.
To compound this effect, policy unpredictability may also emerge in the temporal dimension. While a sequence of intermittent follow-ups of the initial lockdown is highly likely to nip any new spread in the bud, the on/off switch has to be activated by medical evidence (such as the number of people requiring intensive care at a given time), not by fluctuations in public opinion. Perhaps governments may at times be tempted to respond to political cues more than scientific ones.
The negative externalities implied by lack of a coordinated and consistent policy package implies that we might end up in a suboptimal prisoner dilemma-style equilibrium even beyond the medical dimension. Inconsistency and unpredictability would probably lead to erosion of trust both between countries and within them, as citizens alternatively point the finger at their own leaders and their neighbours. Eventually, the alternative to a coordinated, temporary lockdown now might be a prolonged restriction of movements in the future – and not only because of the virus. Irrespective of whether COVID-19 leaves ten thousand or ten million dead, the EU could be among the body count.
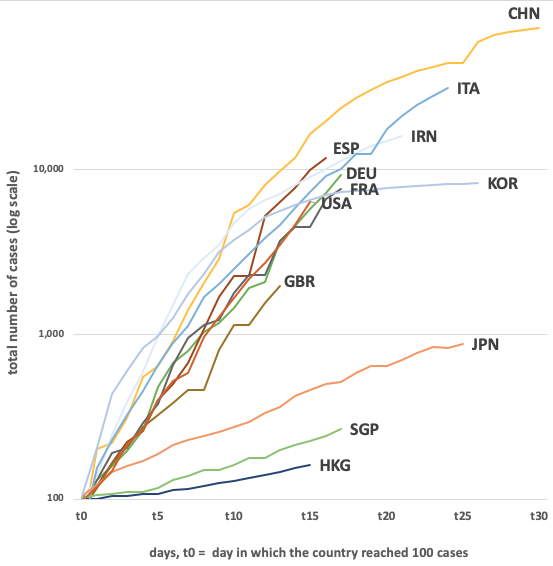
So, is a Europe-wide – or, at least, an EU-wide – simultaneous lockdown the only option? In the short term – say, starting now and for the next few (or not so few) weeks – yes. Business-as-usual policies, all human cost aside, would not be politically sustainable in democracies where information is free, for the reasons expounded above. The case for containment is equally urgent everywhere and the apparently different CFRs across demographically comparable locations should not mislead policymakers. The medical literature (and Figure 1 below) shows that, this early into an outbreak, this is in part a statistical effect due to onset-to-outcome delay – i.e. the time lag between falling ill and either recovery or death (Nishiura et al. 2009, Russell et al 2020) – as well as to wide differences in the extent of testing being conducted and, as a result, of contagion underreporting.
Figure 1 Number of infections in Italy, Hubei (China) and selected OECD countries on 17 March 2020
Notes: t=0 indicates the day in which each country reached about 100 detected cases: 18 January for China, 20 February for Republic of Korea, 22 February for Italy, 25 February for Iran, 29 February for France, Germany and Singapore, 1 March for Spain, 2 March for Hong Kong, 2 March for the US, 4 March for the UK.
Cushioning the short-term costs of the intervention and looking ahead
Any restrictive decisions should not be taken lightly: a lockdown is only feasible if accompanied by appropriate measures to contain economic and social fallout. Both supply and demand suffer a shock. As consumption and production drop simultaneously, the risk of setting off vicious spirals is concrete. Uncertainty over economic policy compounds the effect (Müller 2020). Preserving trust in institutions requires careful tailoring of counterweights.
The guiding principle should be to keep liquidity running (Baldwin 2020). Fiscal measures – ranging from temporary tax cuts to income support and forms of universal basic income (Gentilini 2020) – should be deployed in support of the most heavily hit sectors and areas (Gaspar and Mauro 2020). Measures that keep credit available to firms, such as public guarantees on loans, are of the essence. Some such interventions are already underway in the hardest-hit countries.
At the same time, central banks can provide liquidity in support of bank lending so as to avoid a tightening of credit conditions (Cochrane 2020). As strain in the productive sector piles up on banks’ balance sheets, central banks should also be ready to avert bottlenecks in credit supply (Demertzis et al 2020). Ensuring that smooth market conditions are maintained on the public debt markets with sizable purchases of long-term bonds by central banks, to allow the public sector funding for the necessary support measures and the expenses needed both to upgrade the health system and to support the women and men working on the front line, is of the essence.
A coordinated, simultaneous lockdown can of course only be sustainable if it is temporary. As it is gradually lifted, a comprehensive, well-designed post-emergency policy toolkit should be put in place. The two main pillars of a longer-term strategy to eradicate the virus (as well as likely future pandemics) while resuming economic activity would have to be, first, strengthening the healthcare infrastructure, both human and physical. The response capability of healthcare systems will need to be scaled-up in most countries – for example, ICU availability varies significantly across Europe, in ways that do not always track GDP.10 The second crucial step to undertake amounts to refining our ability to measure and contain virus diffusion, exploiting existing technologies and micro-level data.
In this respect, European policymakers should look at what have proved to be the best practices for epidemic surveillance: testing, contact tracing, isolation of high-risk individuals (based on age or health status) as well as of positive cases (Ferguson et al. 2020). All these measures will need to be implemented in a systematic, consistent fashion while vaccine research proceeds, a cure is found, we develop some form of herd immunity and, hopefully, COVID-19 becomes less aggressive.
Governments should pay special attention to representing this approach correctly to the public and leave no room for suspicion that public health may come at a cost in terms of individual rights.11 Effective containment can be achieved without an iron fist – relying instead on leveraging existing technologies, knowledge and IT diffusion, as well as by mobilising social capital to support voluntary compliance. Europe can use the initial lockdown to get up to speed on these fronts as well as on digital literacy, thus making draconian measures less necessary in the future. The EU’s General Data Protection Regulation provides the right framework to preserve privacy protection.
Looking forward, there seems to be ample room to devise a coordinated strategy to address the threats of pandemics in the longer term. Recent research suggests that social willingness to pay to avoid another COVID-19 in our societies is far above the actual costs needed to greatly reduce its occurrence (Martin and Pindyck 2019, National Academy of Medicine 2016). At the global level, the National Academy of Medicine estimates that an incremental $4.5 billion per year spent on strengthening national public health systems, funding research and development, and on financing global coordination and contingency efforts, would suffice to make the world much safer against pandemics.
As rightly argued in Bénassy-Quéré et al. (2020), the crisis will also represent a test of our ability to develop solidarity. If EU member states manage to unite their efforts in avoiding a ‘common bad’, their cooperation might gain momentum and they might then be able to endow the Union with the crucial common good of a more complete and effective governance. If, instead, they fail on the first basic front, hopes for a deeper economic and political integration might be doomed for a long time.
Authors’ note: The authors of this column are part of the Bank of Italy’s COVID-19 monitoring group. We would like to thank Andrea Brandolini, Pietro Catte, Valerio Ercolani, Maura Francese, Daniele Franco, Eugenio Gaiotti, Giuseppe Parigi, and Michele Savini Zangrandi for helpful comments. The opinions expressed are those of the authors and do not necessarily reflect the views of the Bank of Italy.
References
Anderson, R M, H Heesterbeel, D Klinkenberg and T D Hollingsworth (2020), “How will Country-Based Mitigation Measures Influence the Course of the COVID-19 Epidemic?”, The Lancet.
Baldwin, R (2020), “Keeping the Lights on: Economic Medicine for a Medical Shock”, VoxEU.org, 13 March.
Baldwin, R and B Weder di Mauro, eds (2020), Economics in the Time of Covid-19, A VoxEU.org eBook.
Bénassy-Quéré, A, R Marimon, J Pisani-Ferry, L Reichlin, D Schoenmaker and B Weder di Mauro (2020), “COVID-19: Europe needs a catastrophe relief plan”, VoxEU.org, 11 March.
Cochrane, J (2020), “Coronavirus and Monetary Policy”, in R Baldwin and B Wieder di Mauro (eds), Economics in the Time of Covid-19.
Ferguson, N et al. (2020), “Impact of non-pharmaceutical interventions (NPIs) to reduce COVID19 mortality and healthcare demand”, mimeo, Imperial College.
Gaspar, V and P Mauro (2020), “Fiscal Policies to Protect People During the Coronavirus Outbreak”, mimeo, IMF.
Gentilini, U (2020), “5 Lessons for Using Universal Basic Income During a Pandemic”, Brookings Institution.
Gourinchas, P (2020), “Flattening the Pandemic and Recession Curves”, mimeo, U.C. Berkeley.
Keogh‐Brown, M R, S Wren‐Lewis, W J Edmunds, P Beutels and R D Smith (2010), “The possible macroeconomic impact on the UK of an influenza pandemic”, Health Economics 19(11): 1345-1360
McKibbin, W and R Fernando (2020), “The Global Macroeconomic Impacts of COVID-19: Seven Scenarios”, Brookings Institution.
Müller, H (2020), “COVID-19: Governments Must Avoid Creating Additional Uncertainty”, VoxEU.org, 14 March.
Niehus, R, P M De Salazar, A Taylor and M Lipsitch (2020), “Quantifying bias of COVID-19 prevalence and severity estimates in Wuhan, China that depend on reported cases in international travellers”, preprint available here.
Nishiura H, D Klinkenberg, M Roberts et al. (2009), “Early Epidemiological Assessment of the Virulence of Emerging Infectious Diseases: A Case Study of an Influenza Pandemic”, PLoS One 4.
Pyndyck, R and I Martin (2019), “Welfare Costs of Catastrophes: Lost Consumption and Lost Lives”, NBER Working Paper No. 26068.
Rhodes, A, P Ferdinande, H Flaatten, B Guidet, P G Metnitz and R P Moreno (2020), “The variability of critical care bed numbers in Europe”, Intensive Care Medicine 38: 1647-1653.
Rockloy, J, H Sjodin and A Wilder-Smith (2020), “COVID-19 outbreak on the Diamond Princess cruise ship: estimating the epidemic potential and effectiveness of public health countermeasures”, Journal of Travel Medicine.
Russell, T, J Hellewell, C I Jarvis et al. (2020), “Estimating the Infection and Case Fatality Ratio for COVID-19 Using Age-Adjusted Data from the Outbreak on the Diamond Princess Cruise Ship”, preprint available here.
Tuite, A, V Ng, E Rees and D. Fisman (2020a), “Estimation of COVID-19 Outbreak Size in Italy Based on International Case Exportations”, preprint available here.
Tuite, A, I Bogoch, R Sherbo, A Watts, D Fisman and K. Khan (2020b), “Estimation of COVID-2019 Burden and Potential for International Dissemination of Infection from Iran”, preprint available here.
Tversky A and D Kahneman (1981), “The framing of decisions and the psychology of choice”, Science 30: 453-458
Zhou, F, T Yu, R Du, G Fan, Y Liu, Z Liu, et al. (2020), “Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study”, The Lancet.
Endnotes
1 Key facts on the virus, such as whether it can infect the same individual more than once, have not been established yet. Some drugs have shown promise in treating the disease for a very limited number of patients, but we do not know how well this generalises. Country-level data tell different stories on the case-fatality rate (CFR), i.e. the share of deaths over the number of cases, possibly because of the use of different recording criteria.
2 The literature generally agrees that a two-week quarantine should be enough for most infected subjects to no longer pose a threat to others. However, there is evidence that infectiousness could last a few more days for some, even if they are showing no symptoms (Anderson et al. 2020). Fei Zhou et al. (2020) show that the clinical course of the COVID-19 virus is about 20 days.
3 Other than healthcare, food production and distribution, public security, and so on.
4 This depends on several factors including but not limited to enforcement capabilities of governments, spontaneous response on the part of citizens, and a country’s sociodemographic characteristics.
5 Containment measures halving economic activity for a month and allowing for gradual recovery over a two-month horizon can easily imply a 10% GDP loss on a yearly basis (Gourinchas 2020).
6 Population of European countries (EU and non-EU) as defined by the UN Statistics Division.
7 The latest data from the World Health Organization’s COVID-19 situation dashboard reported a global CFR of 3.8%, but this coefficient is surrounded by a high uncertainty. First, the denominator of a CFR (the number of confirmed cases) is most likely underestimated by up to 60-70% since many of the infected show mild or no symptoms and there is no universal testing (e.g. Niehus et al. 2020, Rockloy et al. 2020, Tuite et al. 2020a, Tuite et al. 2020b). CFRs are therefore overestimated. Moreover, the extent of the overestimation depends on a country’s testing policy – which varies significantly across Europe. This compounds any cross-country differences in the unknown ‘true’ CFRs, depending not on statistical issues but on substantial ones such as demographic structure. Last but not least, not all healthcare systems in Europe would be able to handle a large-scale infection. A certain share of those infected need hospitalization, with the most serious cases requiring admission to intensive care units (ICUs). There is no recent internationally comparable statistic on ICU capacity in different countries, but a study on 2010-2011 (Rhodes et al. 2012) suggests ample cross-country differences. See also https://data.oecd.org/healtheqt/hospital-beds.htm
8 Estimates of time needed to have a vaccine widely available on the market vary, but the consensus is that the testing process – necessary so to avoid side effects that may be more dangerous than the disease – will take at least until the end of 2020.
9 Anecdotal evidence from the Chinese press suggests that COVID-19 may leave some patients unable to fully return to ordinary life even after the infection is gone, on account of lung damage.
10 See endnote 4.
11 In the public debate in Europe, a concern has emerged that epidemic surveillance is not compatible with democratic values and could lead down the slippery slope of digital authoritarianism. This is indeed a risk, but its seriousness depending on how such surveillance is implemented. The GDPR is one of the world’s strictest privacy laws, but provides for exceptions to certain safeguards on public health grounds.