In the absence of efficient vaccines, Europe would face a catastrophic third wave of Covid-19 in the spring of 2021 due to the high transmissibility (Volz et al. 2020) and lethality (Challen et al. 2021) of the British variant. During the winter and in the spirit of the ‘stop-and-go’ strategy, France and many other European countries applied a mild lockdown that was enough to eradicate the historic virus, but not enough to generate a R0 lower than unity for the variant. In a new paper (Gollier 2021), I show that this stop-and-go strategy is a dead end without the exit door of a vaccine. But the slow development of the vaccination campaign in continental Europe raises critical questions. Who should get priority in the vaccination? What is the welfare cost of the delay? How does the presence of ‘anti-vaxxers’ modify the dynamics of the pandemic and the age-structure of mortality risk? And what are the welfare consequences of the currently raging vaccine nationalism?
To answer these questions, I adapted the age-structured SIR model that I developed in Gollier (2020) to explore lockdown and testing strategies. I recalibrated the model with the parameters of the British variant, and I introduced a flexible age-structured vaccination campaign. The initial condition of the SIR dynamics is adapted to the French situation in early January 2021, when the French vaccination campaign started, with an average rate of immunity of 17%. Of course, the results of my model are no more reliable than the assumptions that are made to build it. For example, I assume perfect efficacy of the vaccine, in the sense that, after an average period of three weeks to develop immunity, inoculated individuals cannot develop severe symptoms in case of infection and they cannot transmit the virus. For more details about the structure of the model and its calibration, see Gollier (2021).
Figure 1 Dynamics of the pandemic from day 0 (end of January 2021) in France in the benchmark calibration with 200,000 doses/day and a stop-and-go lockdown strategy
The welfare benefit of speeding the vaccination campaign
In March 2021, France was able to administer 200,000 doses of the vaccine every day, far behind the UK’s speed of vaccination. In my benchmark calibration, I assume that this speed of vaccination is maintained until the end of the year, and that France continues to apply its stop-and-go strategy to control its limited capacity of intensive care units (ICUs). During the first two months of the pandemic, a mild lockdown is maintained, as France vaccinates its most vulnerable segments of the population. But this lockdown is not intense enough – and the vaccination campaign is too slow – to preserve ICU capacity. The model anticipates that France would lose the race between the vaccine and the variant. The stronger lockdown can be relaxed after 40 days. Another wave pops up in the summer as a consequence, but the immunity of the population most likely to occupy ICUs implies that this summer wave does not overwhelm ICUs, in spite of its intensity. The pandemic is erased in the autumn of 2021 thanks to the wider vaccination. Under this scenario, my model estimates that 41,000 middle-aged people and 50,000 senior people will die in 2021, and France will lose 14% of its annual GDP during the first nine months of the year, before a potential rebound in the fourth quarter (outside the time horizon of the model).
What would be the benefit of doubling the speed of vaccination? The death toll would be reduced to 61,000, i.e. by one-third, and the economic loss would go down to 9.3% thanks to the shortening of the lockdown period. There is no doubt that this would be socially desirable, ‘whatever the cost’. Keep in mind that at €30 per vaccination, the economic cost of the vaccination campaign is no larger than 0.1% of annual GDP.
One can also explore the consequence of delaying the vaccination campaign. The doubts that emerged in March about possible side effects (blood clots, thrombosis) of the AstraZeneca vaccine resulted in a suspension of this vaccine for half a week in France and Germany, and for much longer in other countries. The benefit of this suspension remains unknown as I write this column, as the causal link between the inoculation and the symptoms, and the frequency of these side effects, are unclear. The cost of the delay can easily be estimated from the SIR model. A one-week suspension of the entire vaccination campaign in France at the end of March would have increased the dead toll at the end of the pandemic by around 1,800 compared to the benchmark. The economic loss would be increased by €8 billion.
The welfare cost of vaccine misallocation
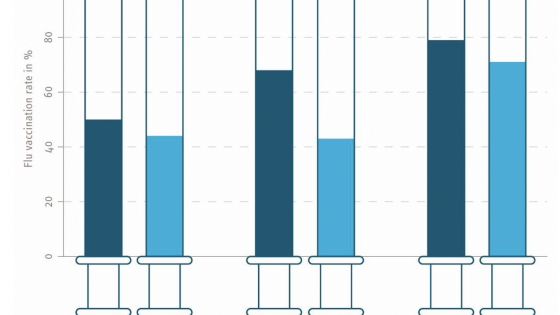
The infection-fatality ratio (IFR) increases exponentially with age, doubling every five years. This means that diverting the priority of the vaccine campaign from older people has an adverse effect on global mortality, but also on the duration and intensity of the lockdown to preserve ICU capacity. There are various possible justifications for departing from the welfare cost minimisation strategy of the vaccination campaign. For example, one may want to compensate essential workers (health workers, teachers, etc.) for their risk exposure. I explore the extreme case where vaccines are allocated on criteria that are independent of mortality risk. In that case, the global death toll is increased by 56,000 compared to the benchmark, with 70,000 more fatalities among the seniors, and 14,000 fewer fatalities among younger people.
The existence of a strong anti-vax movement in France provides another reason for why the allocation of the vaccine will not minimise the welfare cost. Suppose that 30% of the population refuses the vaccine. This would have have several implications. First, many more senior anti-vaxxers will die. But because the virus will circulate more intensely in the senior age class, more senior vaccinated people who are not yet immunised will also die. Because senior people interact much more within their own age class than with other classes, the presence of senior anti-vaxxers implies around 5,000 additional deaths among the senior pro-vaxxer population.
On their side, the anti-vaxxers benefit from the herd immunity built by the vaccination effort of the pro-vaxxers. The presence of the pro-vaxxers in the population will reduce the death toll faced by the anti-vaxxers by 50,000 compared to the situation in which nobody is inoculated – a 35% reduction. This is the positive externality exercised by pro-vaxxers on anti-vaxxers.
Vaccine nationalism offers another illustration of the misallocation of the vaccine. Under the veil of ignorance, it is inefficient to inoculate a young British citizen before a senior German one. To simulate the impact of this form of nationalism, I examine a model with two identical Frances: one without any vaccine capacity, and another one with a capacity to administer 400,000 doses per day. I compare the first-best solution in which this capacity is equally shared by the two countries to the nationalistic solution in which the producing country inoculates its entire population before exporting the vaccine to the other country. Vaccine nationalism increases the global death toll by 20%. The economic damage in the importing country is more than twice its equivalent in the producing country. And the death toll at the end of the pandemic is more than 150% larger in the importing country. Given the large discrepancy between the intensities of the health and economic crises incurred by the producing and importing countries, it is illusory to expect any politically acceptable cooperation to allocate the vaccine capacity efficiently at the international level, in spite of the efforts of the World Health Organization (through COVAX).
References
Challen, R, E Brooks-Pollock, J M Read, L Dyson, K Tsaneva-Atanasova and L Danon (2021), “Risk of mortality in patients infected with SARS-CoV-2 variant of concern 202012/1: matched cohort study”, The British Medical Journal 372: n579.
Gollier, C (2020), “Cost-benefit analysis of age-specific deconfinement strategies”, Journal of Public Economic Theory 22(6): 1746-1771 (pre-published in Covid Economics 24: 1-31).
Gollier, C (2021), “The welfare cost of vaccine misallocation, delays and nationalism”, Covid Economics 74: 1-24.
Volz, E et al. (2020), “Transmission of SARS-CoV-2 lineage B.1.1.7 in England: Insights from linking epidemiological and genetic data”, medRxiv 2020.12.30.20249034.
Endnotes
1 In France, the AstraZeneca vaccine represented approximately half of the vaccination capacity at the time of the suspension.