Existing research has found negative short-term consequences of the COVID-19 pandemic on mental health (e.g. McGinty et al. 2020, Pierce et al. 2020, Pan et al. 2021, Wang et al. 2021), but the longer-term effects have been less documented (e.g. Salanti et al. 2021). People may have developed better coping strategies, or the accumulated effects of stress may make longer-term effects more severe than the short-term effects.
In a recent paper (Hvide and Johnsen 2021), we provide novel evidence on the longer-term effects of the pandemic on mental health, using near real-time register data covering the universe of general practitioner (GP) consultations in Norway until the end of 2020 to address this issue – in all about 14 million consultations.
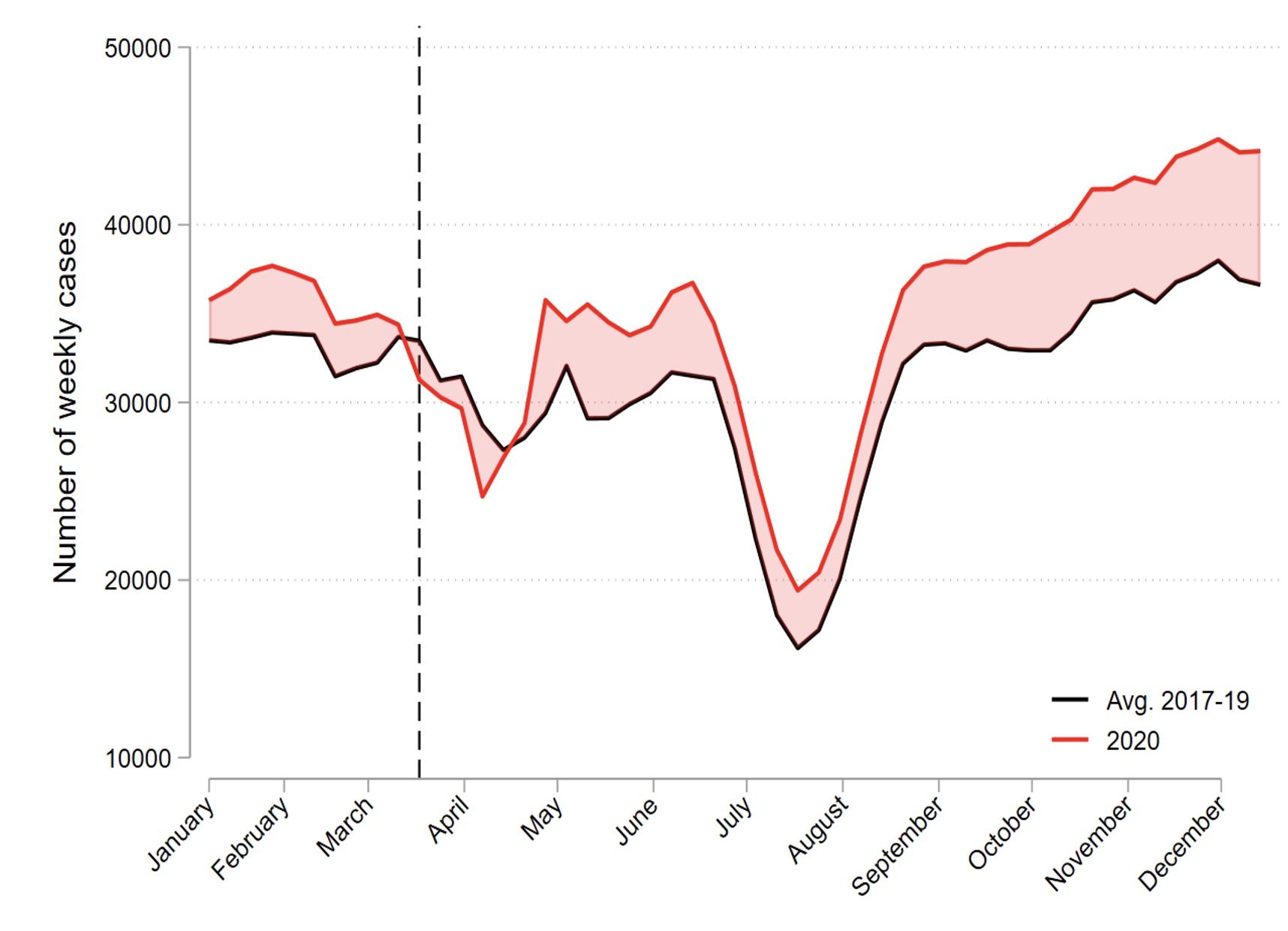
Figure 1 shows that the number of GP visits related to mental health diagnoses was high relative to prior years in late spring and early summer of 2020, consistent with evidence from other countries (cited above), but those numbers fell back towards pre-2020 levels during July and August. Our main finding is an acceleration of cases starting in September 2020 and still present at the end-of-year. The increase in cases is large – we estimate that the weekly number of mental health cases in the autumn of 2020 was 17% larger than the 2017–19 average. At a per-capita level, the increase in weekly cases relative to prior years was about 1 per 1,000 people in July–August, and doubled to 2 per 1,000 in December. This acceleration in mental health cases during the autumn of 2020 suggests that the accumulated effects of stress in the period outweighed the development of better coping strategies in the population.
Figure 1 Weekly number of mental health cases in 2020 (black) versus the 2017–2019 average (red)
Note: A ‘mental health case’ is a GP consultation that resulted in a psychological diagnosis.
As Norway had a low incidence of COVID-19 cases and deaths during the autumn of 2020 compared to many other countries, it seems plausible that the acceleration in mental health cases during the period was due to the accumulated effects of lockdowns and movement restrictions, rather than from stress due to fear of infection.1 As lockdowns and movement restrictions have been a policy response to the pandemic worldwide, our findings should be of interest to policymakers in many countries contemplating the difficult trade-offs of continued lockdown policies. Our findings also have broader interest by providing detailed population-level documentation of the mental health effects of prolonged shutdowns and limits to social interaction.
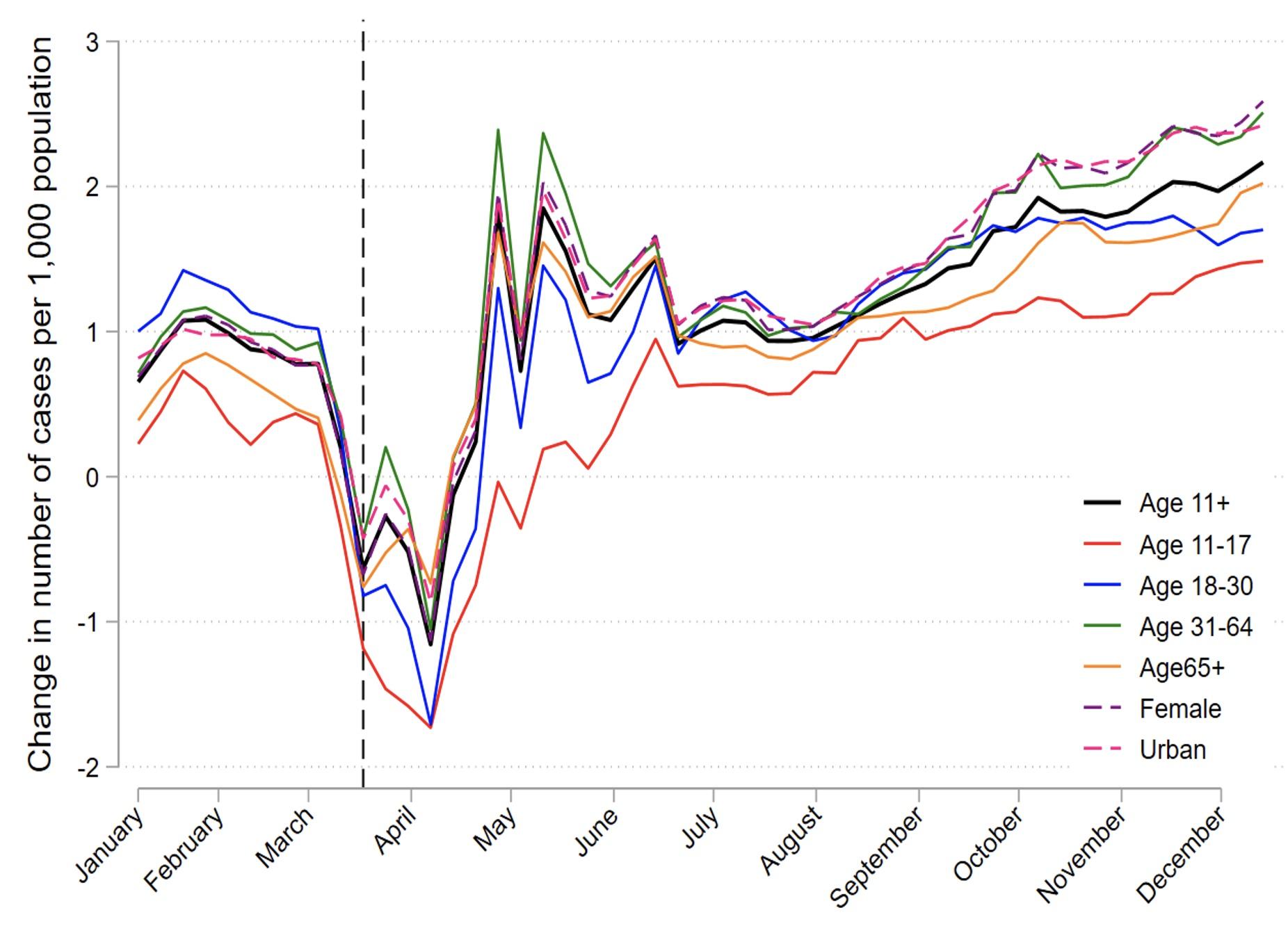
Figure 2 considers the increase in cases for different subpopulations. To make the numbers comparable across sub-populations, we compute the increases in the number of cases in 2020 relative to the 2017–19 average at a per capita level. The main cities have been hubs for COVID-19 cases and lockdowns, as have many metropolitan areas globally. As shown in Figure 2, these urban areas experienced larger increases at the per-capita level in mental health cases during September–December than more rural areas. The increases were also large for females. While the per-capita increase was lowest for adolescents (aged 11–17), this age group actually experienced the largest percentage increase relative to other groups.
Figure 2 The increase in weekly number of mental health cases in 2020 versus 2017–2019 average for subpopulations, per 1000 capita subpopulation
Note: ‘Population’ on the y-axis refers to the number of individuals in the subpopulation that attended a GP in 2020.
As can be seen in Figure 1, the number of mental health cases in Norway was unusually high in January 2020, and we are not aware of any institutional changes that could explain the spike. One explanation could be that the unusually foul weather in January 2020 led to a ‘lockdown’ created by nature.2 In our paper, we control for a possible ‘2020 effect’ unrelated to COVID-19 by comparing the increase in average weekly cases during weeks 40–51 in 2020 to the corresponding increase during weeks 1–10 of 2020 (i.e. prior to the outbreak). The estimate from this approach implies that the extra increase in P-cases during weeks 40–51 in 2020 was substantial, at 9%.
As can be seen from Figure 1 (black line), Norway faces a ‘long winter’ effect, in that the number of mental health cases typically increases during the autumn months (Øverland et al. 2020), possibly due to lack of exposure to the sun (Lambert et al. 2002). To investigate whether the long winter effects interact with the COVID-19 effects, we analysed the increases in mental health cases for the three northern-most counties (Nordland, Troms, and Finnmark) where populations live close to or above the arctic circle. The percentage increase in mental health cases for these counties was about 9%, which is lower than the increase for the overall population. This suggests that the long winter effects are not driving our results.
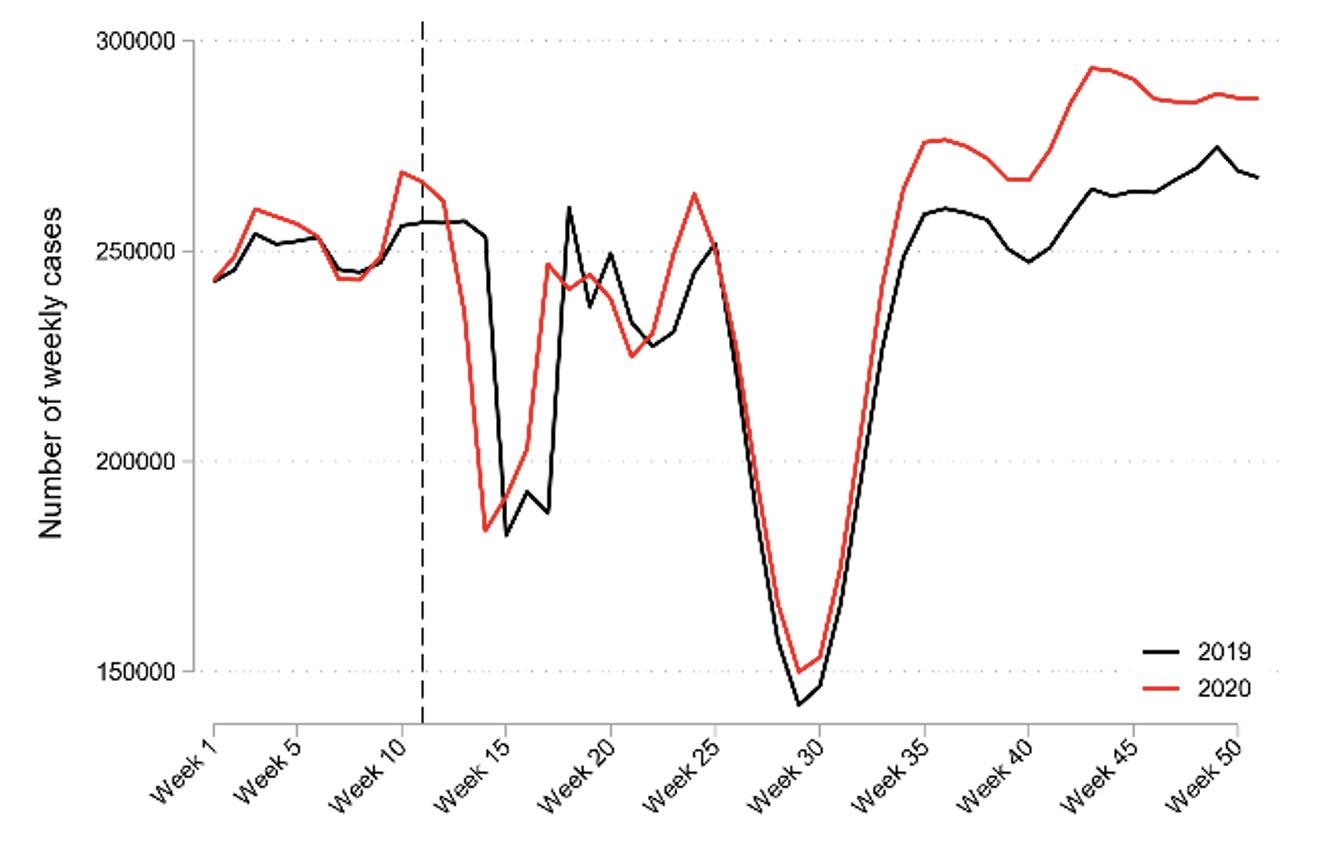
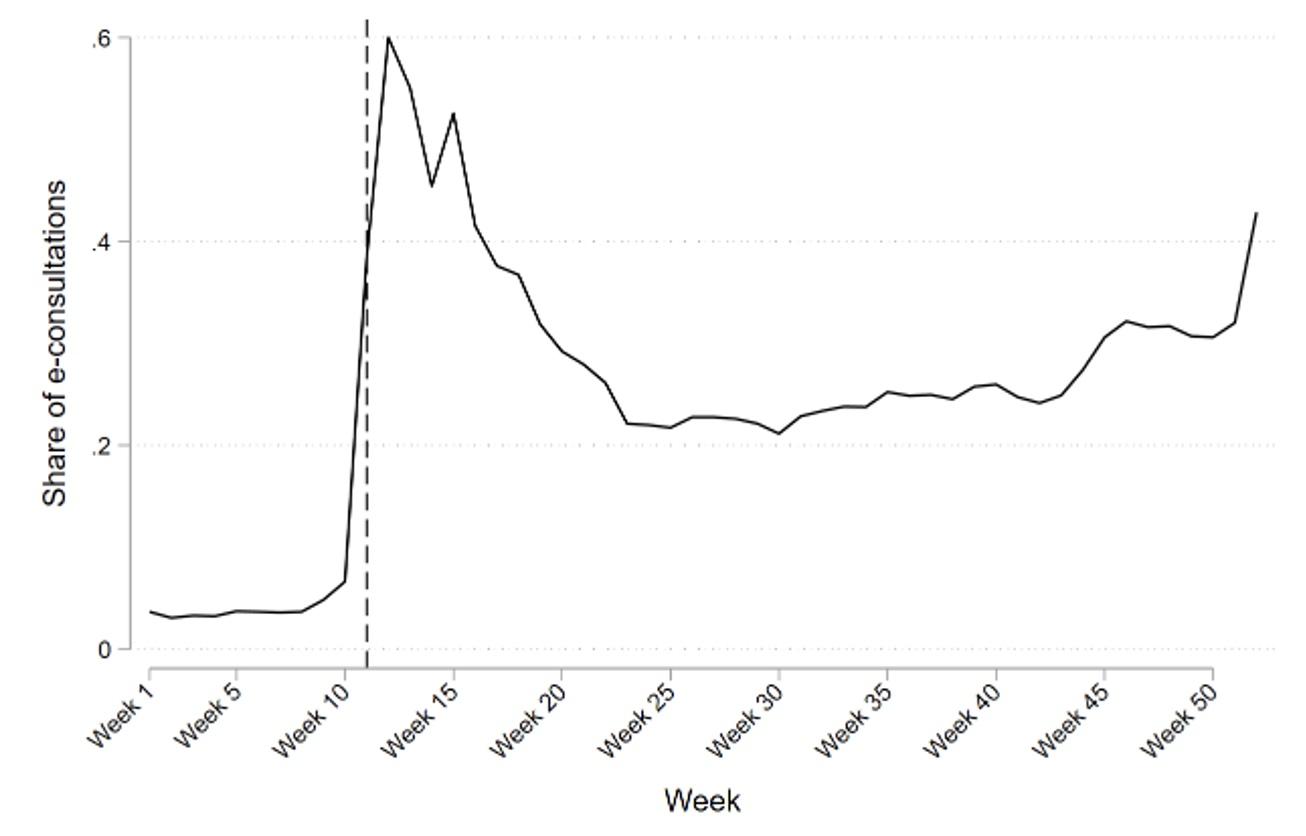
Finally, it should be noted that the Norwegian setting provides data uniquely suited to studying population-level effects of COVID-19 on health issues. Many countries experienced a large drop in GP encounters around the outbreak of the COVID-19 pandemic relative to prior years (see Mansfield et al. 2021 for the UK and Holland et al. 2021 for the US). This drop did not occur in Norway, as shown in Panel A of Figure 3. The reason was a fast transition to electronic online encounters, as shown in Panel B of Figure 3.3
Figure 3 Weekly GP encounters did not drop in Norway after the pandemic due to a fast transition to online consultations.
A. Weekly GP encounters in 2020 vs 2019
B. Share of online consultations
References
Holland, K M et al. (2021), “Trends in US emergency department visits for mental health, overdose, and violence outcomes before and during the COVID-19 pandemic”, JAMA Psychiatry, published online 3 February.
Hvide, H K and J V Johnsen (2021), “COVID-19 and Mental Health: a Longitudinal Population Study from Norway”, CEPR Discussion Paper 16195.
Lambert, G W et al. (2002), “Effect of sunlight and season on serotonin turnover in the brain”, The Lancet, 360(9348): 1840–1842..
Mansfield, K E et al. (2021), “Indirect acute effects of the COVID-19 pandemic on physical and mental health in the UK: a population-based study”, The Lancet Digital Health, 3(4): e217–e230.
McGinty, E E et al. (2020), “Psychological distress and loneliness reported by US adults in 2018 and April 2020”, JAMA 324(1): 93–94.
Pan, K Y et al. (2021), “The mental health impact of the COVID-19 pandemic on people with and without depressive, anxiety, or obsessive-compulsive disorders: a longitudinal study of three Dutch case-control cohorts”, Lancet Psychiatry 8(2): 121–129.
Pierce, M et al. (2020), “Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population”, Lancet Psychiatry 7: 883–92.
Salanti, G et al. (2021), “An efficient way to assess the effect of COVID-19 on mental health in the general population”, Lancet Psychiatry, published online 16 March.
Wang, Y et al. (2021), “The impact of quarantine on mental health status among general population in China during the COVID-19 pandemic”, Molecular Psychiatry, published online January.
Øverland, S et al. (2020), “Seasonality and symptoms of depression: A systematic review of the literature”, Epidemiology and Psychiatric Sciences 29.
Endnotes
1 Source: Our World in Data (https://ourworldindata.org/coronavirus/country/norway).
2 January 2020 was the wettest January on record in Norway (e.g. https://kommunikasjon.ntb.no/pressemelding/januar-2020-ble-den-vateste-noen-gang?publisherId=17846853&releaseId=17878908).
3 The homepage of The Norwegian Medical Association contains additional information on the GP refund arrangement, and the transition to electronic consultations during 2020 in Norway (https://normaltariffen.legeforeningen.no/book/Fastlegetariffen-2020/m-02).