“Economics of Mobilization and War” was the title of my father’s first publication as an assistant professor of economics at Harvard (Baldwin et al. 1952). The book analysed the socioeconomic trade-offs facing America during the Korean war – a war that was brutal, but not the sort of ‘total war’ where trade-offs are waved off. The 1952 analysis holds surprising relevance to today’s crisis – although perhaps it shouldn’t be surprising.
The world is at war with COVID-19, but ‘World War COVID” this is not ‘total war’. As was true during the early stages of the Korean War, no one knows how big the COVID combat will end up being. That means that governments are having to perform balancing acts.
Many economic analysts approach these balancing acts using cost-benefit analyses that weigh the value of human lives saved against the economic losses arising from lockdowns and other containment policies. Gollier and Straub (2020) write, when discussing the usefulness of containment, that “the economic and social cost is going to be severe … How can we compare €250 billion to a million deaths?” Likewise, many cite Correia et al. (2020), who argue that containment during the Spanish Flu didn’t cost dollars but actually made dollars (in the medium run). Both sets of authors implicitly embrace the standard cost-benefit analysis.
This column suggests an alternative approach to thinking about the balancing acts – an alternative that has been used in wartime.
Trade-offs in wartime
In the 1952 book, none of the authors calculated the GDP loss per soldier saved involved in shifting civilian production to military production. The approach was to think about how to ‘achieve the necessary’ while doing as little damage as possible to society’s socio-politico-economic fabric.1 In economic jargon, it was an approach of constrained optimisation.
As in wartime, I believe the challenge today should be framed as a constrained optimisation, but today there are two constraints – a medical constraint and a tolerability constraint. Moreover, the balancing, in my view, is not between deaths and dollars; it is between infection rates on one hand, and the tolerability of containment policies on the other hand … The mission-critical task today is to develop a strategy for remobilising workers without risking a medical overload.
As in wartime, I believe the challenge today should be framed as a constrained optimisation, but today there are two constraints – a medical constraint and a tolerability constraint. Moreover, the balancing, in my view, is not between deaths and dollars; it is between infection rates on one hand, and the tolerability of containment policies on the other hand.
To keep containment policies tolerable, remobilisation of the workforce is necessary. Stockpiles and inventories will eventually run low. At that point, financing expenditure on goods that don’t exist will backfire (Baldwin 2020c). What this means is that maintaining a high level of consumption – a key component of maintaining high levels of tolerability – will eventually require remobilisation of some workers. The mission-critical task today is to develop a strategy for remobilising workers without risking a medical overload.
The COVID containment ‘stringency possibility corridor’
A vaccine will defeat COIVD-19 in a year or two, but current containment policies are too disruptive to maintain until then. That’s the problem. That is the dilemma.
- On one hand, governments need to sufficiently contain social interactions to ensure that COVID-19 spreads slowly enough to avoid overloading the healthcare system.
The reason is simple. Overloaded hospitals can’t provide patients with the best possible care. Lots of people are going to die from COVID no matter what; more will die than need be if hospitals are deluged.
- On the other hand, governments cannot ask the impossible of their citizens; peoples’ tolerance of containment is not infinite.
People will tolerant losses in wellbeing for short periods, especially when it is in the name of a good cause. But If the wellbeing losses are too great for too long, people will simply ignore them or cheat on them in unpredictable ways. If the implied wellbeing losses involve hunger and/or outrageous inequalities, the intolerance could manifest itself quickly and chaotically – as I argued in my Vox column from three weeks ago (Baldwin 2020b).
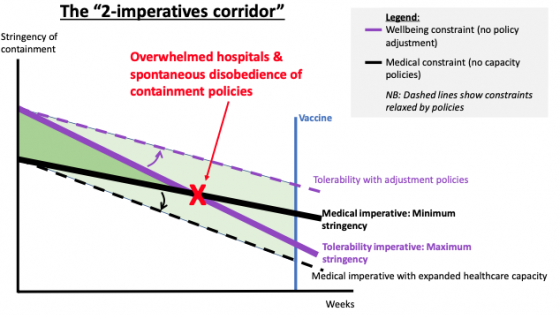
These two imperatives – the medical imperative and the tolerability imperative – can be conceptualised as creating a ‘corridor’ for the stringency of containment policies (Figure 1).
- The medical-imperative constraint (heavy black line) defines the minimum stringency.
It’s downward sloped for two reasons: expanding hospital capacities, and incremental ‘herd immunity’. First, as hospital capacities expand, the society can deal with a higher rate of infection without sacrificing healthcare quality (more on this below). Second, the rate of infection falls along with the share of the population that is susceptible (more on this below), so as time passes and more people have recovered or perished from COVID-19, any given stringency level will produce a lower infection rate.
- The wellbeing imperative (heavy purple line) defines the maximum tolerable stringency.
It falls over time for two reasons. First, suppressed consumption and socialising mounts with time as people get fed up with the sacrifices. Second, containment policies directly reduce the economies output of goods and services, so shortages will begin to appear as stockpiles and inventories run low.
These constraints are not things that are easily quantified – although epidemiologists and public health specialists have attempted to model the medical constraint (e.g. Ferguson 2020). The tolerance constraint is much harder to quantify, but it is something that is very much in the minds of politicians around the world.
Figure 1 Two imperatives define the containment stringency ‘possibility corridor’
Source: Author’s elaboration. Lines are drawn as linear for drafting convenience.
As drawn, the ‘stringency possibility corridor’ shows the pessimistic – but possibly realistic – case where today’s containment policies cannot be maintained. There is no pathway that takes us from today to the vaccine without violating at least one imperative. When the minimum medical demands exceed the maximum tolerance (as they do at the red “X”), things fall apart. Civil disobedience undermines containment policies, and the result is overwhelmed hospitals (after a lag).
As drawn, the ‘stringency possibility corridor’ shows the pessimistic – but possibly realistic – case where today’s containment policies cannot be maintained. There is no pathway that takes us from today to the vaccine without violating at least one imperative. When the minimum medical demands exceed the maximum tolerance (as they do at the red “X”), things fall apart. Civil disobedience undermines containment policies, and then result is overwhelmed hospitals (after a lag).
If this is indeed the situation, governments will have to find ‘constraint-relaxing policies’ that move the minimum and/or the maximum to create a viable pathway that stretches to the vaccine’s widespread deployment. These are schematically illustrated with the dashed purple and dashed black lines.
The first step towards thinking ahead about such constraint-relaxing policies is to consider the underlying logic of the constraints in more detail.
The medical constraint/imperative
While it is widely understood that lockdowns save lives in advance economies, the ‘structural model’ behind that conclusion is worth clarifying. It turns on three facts and two deductions.
- Fact #1: COVID-19 is explosively infectious, with one sick person infecting something like two to three people in the early stages of the epidemic (or maybe higher; Sanche 2020).
This is why, as Dr Ashish Jha, Director of the Harvard Global Health Institute, put it: “Some of the best epidemiologists in the world are estimating that between 40% and 70% of adults will end up getting an infection.”
- Fact #2: COVID-19 is a killer.
Doctors tell us that it has a death rate of somewhere in the low single digits when patients are properly cared for (WHO 2020). This is why a large number of people are going to die with or without containment policies.
- Third, the death rate is much higher when patients cannot be properly cared for – as was the case in Wuhan, China and Bergamo, Italy.
The conclusion is obvious. Containment policies do not save lives directly, they save lives by reducing the chance that hospitals are overrun. It is the limits of hospital capacity – in particular the stock of ICU beds, personal protective equipment (PPE) for medical staff, respirators for patients, and the like – that create the medical imperative.
In a nutshell, COVID-19 will kill many people, but it will kill more if healthcare systems are stretched beyond capacity. The medical imperative is to avoid the avoidable deaths.
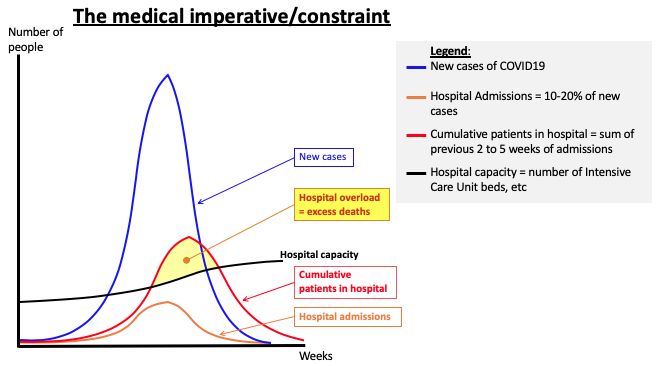
Figure 2 Hospital capacity and the medical imperative.
Note: Flattening the epidemiological curve is not about saving lives directly, it is about avoiding calamity at the hospitals that results in sub-par treatment which, in turn, result in more deaths than necessary.
Source: Author’s elaboration based on diagrams on WHO.int.
Figure 2 shows the well-known epidemiological (epi for short) curve (the blue bell-shaped curve) that plots the number of new cases against time. As explained on many websites, the number of new cases first rises explosively, then peaks, and then decelerates rapidly (for an economist’s view of the logic of the epi curve, see my Vox column from four weeks ago, Baldwin, 2020a).
Recent medical studies (e.g. Sanche 2020) report that only a fraction of those who get the disease will require hospitalisation, something like 5-20%. The orange bell-shaped curve shows the fraction of new cases who are admitted to hospitals. Medical literature reports that the typical hospital stay is a matter of weeks, so the cumulative number of COVID-19 patients (the red bell-shaped curve) in the hospitals piles up – that is why the ‘cumulative patients in hospital’ curve has a higher peak that is delayed.
The cumulative-patients curve is the critical one. If it exceeds hospitals’ capacity (shown as the black line), more patients will die than if the capacity had not been exceeded.
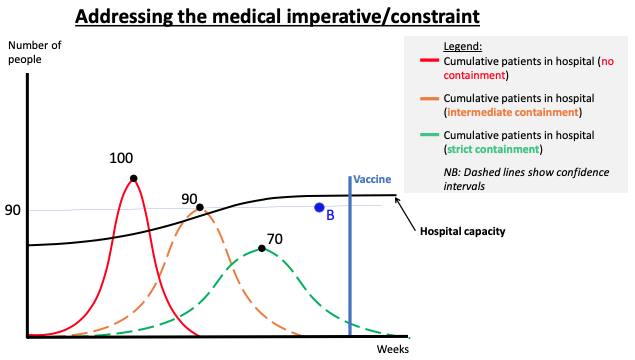
Figure 3 Meeting the medical imperative by flattening the epi curve.
Source: Author’s elaboration.
Figure 3 shows the original cumulative-patients curve (solid red curve) from Figure 2 with two more cumulative-patients curves added. The orange curve illustrates the impact of containment policies of intermediate stringency, while the green curve illustrates it for strict containment policies. As before, the black line shows the hospital capacity constraint over time. As this illustration is drawn, medical constraint is violated without containment politics (red curve). With intermediate containment policies (orange curve), the overload is reduced but not eliminated. Stricter measures (green curves) set the probably of overload to zero.
Importantly, the intermediately stringent containment policies are not good enough in the early weeks of the pandemic. But once the hospital capacity has expanded sufficiently – say, point B – then the intermediate policies are sufficient. The intermediate policies lead to a maximum of, say, 90 (where the index of 100 is the cumulative patients with no containment policies). This shows one reason why the medical imperative can be met with successively less stringent containment policies as time passes. (This assumes that the surge capacities of hospitals are being expanded, as they are in most rich nations.)
The wellbeing constraint/imperative
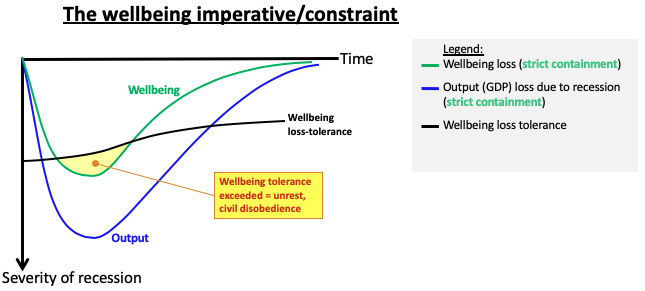
A similar analysis shows the constraints on the tolerability of containment policies. The key point to keep in mind is that stricter containment policies lead to deeper recessions (Gourinchas 2020). This is why stringency of containment policies are linked to the tolerability of containment policies.
The diagram shows the ‘recession curve’ (blue Nike swoosh) which is caused by the pandemic and – especially – by the containment policies (Baldwin and Weder di Mauro 2020a). The green curve illustrates wellbeing, broadly defined (and roughly correlated with consumption). The black curve exemplifies what peoples’ tolerance for wellbeing loss might be. It is rising since tolerance has a ‘sell by’ date – people get antsy, discontent accumulates, and the reduced production means that the range of available goods shrinks, and prices rise.
The yellow area in the diagram suggests that if the containment policies are strict enough, so that the recession is deep enough, the loss of wellbeing will exceed people’s tolerance. The tolerance constraint falls (i.e. they can tolerate less loss) over time as people’s impatience with the sacrifices rise. The result in the best of cases is widespread cheating on the restrictions. If lockdown policies eventually lead to reduced food production/ delivery and people go hungry or worse, tolerance could evaporate very quickly.
Figure 4 The wellbeing constraint
Source: Author’s elaboration.
Solving the dilemma by bending the constraints
What should government do? The key is to think hard about the two imperatives – the medical imperative and the tolerability imperative – and find means of bending both constraints in ways that keep the corridor open, to ‘widen the corridor’ as it were (as illustrated by the small arrows in Figure 1). Governments need to focus on relaxing both constraints to ensure that they can keep control of the situation.
Testing will help bend both constraints in the right direction. As Dewatripont et al. (2020) argued, testing is a key to remobilising the workforce while maintaining a sufficiently low infection rate. As I argued in Baldwin (2020c), testing is also the key to relaxing the medical imperative for the second wave of disease that many epidemiologists think is coming.
Exactly what needs to be done to relax the constraints will require a great deal more detailed work by area experts on the economic side and doctors on the medical side. On the economic side it is mostly about substitutes, complements and protection. On the medical side it’s about clever ways to reduce the infection rate while allowing more workers to get back to work. I’ll address some of the economic aspects of this in future VoxEU columns.
Concluding remarks
Current containment policies are, I would argue, too disruptive to maintain until 21st century tools like vaccines come along. This is the problem. It is a two-constraints problem. The two constraints dictate a ‘stringency possibility corridor’ between two imperatives. Containment policies must be stringent enough to avoid the human tragedy of overwhelmed hospitals, but lax enough to avoid exceeding citizens’ tolerance for loss of wellbeing. Solving the dilemma will require an increase in production and relaxation of constraints – in short, it will involve a partial remobilisation of the workforce.
Current containment policies are, I would argue, too disruptive to maintain until 21st century tools like vaccines come along. This is the problem. It is a two-constraints problem. The two constraints dictate a ‘stringency possibility corridor’ between two imperatives. Containment policies must be stringent enough to avoid the human tragedy of overwhelmed hospitals, but lax enough to avoid exceeding citizens’ tolerance for loss of wellbeing. Solving the dilemma will require an increase in production and relaxation of constraints – in short, it will involve a partial remobilisation of the workforce.
Of course, the most obvious set of constraint-bending policies are already being implemented by all advanced economies. Governments are making the lockdowns more tolerable by launching vast economic packages that shield the incomes of the most vulnerable while shielding jobs, firms, banks and networks from permanent harm. The guiding thought today is: Go big. Act fast. Keep the lights on.
That was the right approach in the first stage of the pandemic. It basically accepted that a massive recession is an unavoidable public health measure. But the choices going forward will require a different type of thinking – one that focuses on bending the constraints, not just bending the epi curve.
In my next column, I’ll use the notion of the ‘stringency possibility corridor’ to discuss the many remobilisation plans, which are sometimes labelled (optimistically) as ‘exit’ plans. These include those that involve intermittent application, gradually fading stringency, stringency varied by sector, by worker, by age, by location, by job, and so on.
References
Baldwin, R and B Weder di Mauro, eds (2020a), Economics in the Time of COVID-19, a VoxEU.org eBook, CEPR Press.
Baldwin, R and B Weder di Mauro, eds (2020b), Mitigating the COVID economic crisis: Act fast and do whatever it takes, a VoxEU.org eBook, CEPR Press.
Baldwin, R (2020a). “It’s not exponential: An economist’s view of the epidemiological curve,” VoxEU.org, 12 March 2020.
Baldwin, R (2020b). “Inequality and pandemic make an explosive mix,” VoxEU.org, 15 March 2020.
Baldwin, R (2020c). “The supply side matters: Guns versus butter, COVID-style,” VoxEU.org, 22 March 2020.
Correia, S, S Luck, and E Verner (2020). “Pandemics Depress the Economy, Public Health Interventions Do Not: Evidence from the 1918 Flu.” Mimeo.
Ferguson, N M, D Laydon, G Nefjati-Gelani et al. (2020), “Impact of non-pharmaceutical interventions (NPIs) to reduce COVID-19 mortality and healthcare demand”, Imperial College COVID-19 Response Team.
Gollier, C and A Straub (2020). “Some micro/macro insights on the economics of coronavirus. Part 2: Health policy,“ VoxEU.org, 03 April.
Gourinchas, P-O (2020). “Flattening the pandemic and recession curves,” Chapter 2 in R Baldwin and B Weder di Mauro (eds), Mitigating the COVID economic crisis: Act fast and do whatever it takes, a VoxEU.org eBook, CEPR Press.
Sanche S, Y T Lin, C Xu, E Romero-Severson, N Hengartner and R Ke (2020), “High contagiousness and rapid spread of severe acute respiratory syndrome coronavirus 2”, Emerging Infectious Diseases.
US Office of Defense Mobilization (1951), Report to the President by the Director of Defense Mobilization. Washington, DC.
WHO (2020), Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19), February.
Endnotes
1 This reasoning is explicit, for example, in the Director of Defense Mobilization’s 1951 report to the President, page, cited in Baldwin et al (1952: 5).