COVID-19 has claimed over 600,000 lives worldwide and has imposed unprecedented economic damage (World Health Organization 2020). Though virtually no country was spared by the pandemic, its impact has varied considerably across countries, with some managing to respond much more effectively than others. Some studies have investigated what factors may explain these differences, from the adoption of different policies (Hsiang et al. 2020, Fang et al. 2020 and references therein) to cultural factors that may have contributed to the success of social-distancing measures (Barrios et al. 2020, Durante et al. 2020a, 2020b, Giuliano and Rasul 2020).
One aspect that remains relatively unexplored concerns how the virus spread across space from the first limited outbreaks to entire countries, and, in particular, the role that internal migration may have played in this context. Extensive anecdotal evidence and news reports indicate that, following the early outbreaks and the subsequent economic slowdown, many internal migrants decided to return to their place of origin. This was especially true for recent migrants who maintain strong ties with their place of origin but have a limited support network in the destination place. In some cases, the decision to ‘return home’ was prompted by the announcement by local authorities of the imposition of ‘red zones’ and other mobility restrictions (Giuffrida and Tondo 2020).
In principle, the return of migrants to their hometowns from places heavily hit by the pandemic may have contributed to the spread of the virus since these individuals could have been asymptomatic carriers or may have contracted the disease while travelling. This could ultimately result in places with more returning migrants experiencing more COVID-19 cases and deaths. However, no systematic evidence exists about the plausibility and importance of this channel.
In a recent working paper (Valsecchi and Durante 2020), we attempt to fill this gap by investigating the relationship between internal migration and the spread of COVID-19. We focus on Italy, one of the countries most affected by the pandemic and traditionally characterised by considerable flows of internal migrants, most notably from southern to northern regions.
We exploit the fact that, after the first outbreak of COVID-19 in late February, most cases were concentrated in a small number of provinces in the regions of Lombardy, Veneto, and Emilia-Romagna.1 Using comprehensive data on the place of origin and destination of individuals having migrated over the previous years, we construct a measure of the potential for return migration from early-outbreak areas to each province. We then examine whether provinces with more migrants potentially returning from outbreak areas experienced a higher number of COVID-19-related deaths and higher total excess mortality over the ensuing months.
One key aspect of our analysis is that we use information on migration patterns that pre-date the COVID-19 pandemic and cannot therefore be affected by the latter. Another important element is that we exploit differences between provinces in the number of migrants to specific areas that were affected by the pandemic earlier on, controlling for total outmigration. This alleviates possible concerns that a particular characteristic of the province of origin (e.g. local institutions, health capacity, and civic capital) may drive both migration and COVID-19 mortality.
Furthermore, to rule out the possibility that our findings are driven by a generic North-South divide, we compare the evolution of COVID-19 mortality between provinces of the same region. Our main outcome of interest is the number of deaths due to COVID-19, which is available for each province in each month. However, to alleviate the concern that COVID-19 deaths may be misreported or underestimated, and that this bias may differ between provinces (Ciminelli and Garcia-Mandicó 2020a, 2020b), we also consider the evolution of total (excess) mortality. This allows us to test the effect of return migration on the total number of deaths relative to those recorded in the same month of previous years.
Finally, to shed light on the mechanism through which return migration influences the spread of COVID-19, we exploit data on actual mobility between provinces in the months before and after the national lockdown. These high-frequency data are based on phone-tracking records and provide a clear picture of the total number of daily displacements between outbreak areas and any province from which migrants originate.
Key results
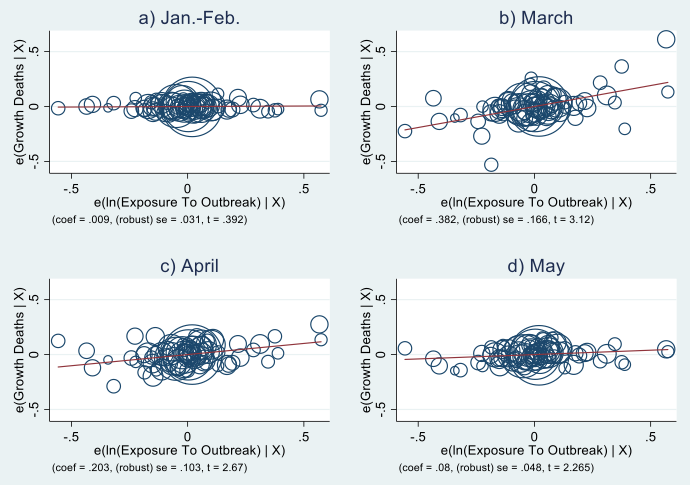
We first look at the effect of potential return migration from outbreak areas on total (excess) mortality in provinces other than those concerned by the initial outbreaks. In Figure 1, we plot the statistical relationship between the two variables separately for the months of January–February (pre-pandemic), and March, April, and May (post-pandemic).2 Each circle represents a province, with larger ones representing more populated provinces. All regressions include regional dummies and a wide range of controls at the province level.3
Figure 1 Exposure to outbreak and growth of total deaths by province-month
Notes: Relationship between growth of total deaths per province and ln(Exposure To Outbreak) partialled out of region FEs and province controls. Circles represent province population.
Panel (a) clearly shows that, prior to the beginning of the pandemic, there is virtually no relationship between potential return migration from outbreak areas and total mortality. The relationship becomes positive and significant, instead, in March, when the virus starts spreading to the rest of the country, and remains so in April and May though weakening gradually. This pattern is consistent with the overall evolution of COVID-19 cases and deaths in the country, which peaked between March and April and declined in May. The effect is sizeable: a 50% increase in potential return migration from outbreak areas relative to the mean is associated with 147 additional total deaths per province.
We calculate that, if all provinces had a potential return migration equal to that of the province at 10th percentile of the distribution, they would have experienced 7,348 fewer total deaths and 5,895 fewer COVID-19 deaths. This corresponds to 60% of all COVID-19 deaths in non-outbreak regions, and to 18% of all COVID-19 deaths in the country.
We then explore to what extent the link between potential return migration and incidence of COVID-19 actually operates through an increase in mobility from outbreak areas to migrants’ hometowns. Figure 2 shows how the effect of potential return migration on mobility evolves, between the end of January and the end of April. The graph shows a clear and significant increase in mobility in the two weeks between the first outbreak and the lockdown, which is consistent with migrants returning to their place of origins before the national lockdown and with the timing of the effect on COVID-19 deaths documented above. Additional calculations (in the paper) suggest that increased mobility between outbreak areas and migrants’ hometowns accounts for most of the effect on mortality documented in Figure 1.
Figure 2 Exposure to outbreak and trips from outbreak areas by province-week
Notes: The figure is based on a regression of the Inverse Hyperbolic Sine of the number of trips from outbreak areas (per 1,000 inhabitants) on exposure to outbreak interacted with week dummies, date FEs, region-week FEs, and the province controls (interacted with week dummies). Dashed lines represent 95% confidence intervals. Dates on the x-axis indicate the beginning of the week.
Concluding remarks
The evidence emphasises the potential role played by internal migration in the context of a pandemic. Previous work has shown that, by reinforcing economic connections between different areas of a country, internal migration can boost aggregate productivity (Bryan and Morten 2019), help dissipate local negative economic shocks (Monras 2018), and let migrants’ households at origin diversify risks (Gröger and Zylberberg 2016). Our results indicate that the opposite may apply to the case of health shocks: they may propagate shocks and constitute an additional risk for households in migrants’ hometowns.
While the issue of international migration and the necessity to close the frontiers to prevent the further spread of the virus has attracted vast political debate, the discussion on how to deal with internal migration has been rather limited, arguably due to the difficulty, both logistical and political, of imposing long-lasting restrictions to mobility within a country.
An alternative and less invasive approach would be for governments to keep up-to-date databases of migrants, particularly recent ones, to be in the position, when a new outbreak occurs, to reach out to them to raise awareness of the risks of travelling for themselves, their families, and the community at large. Information on migration-related connections between provinces could also be used by policymakers to predict what areas of the countries a health emergency may likely extend to and to allocate public medical and economic resources accordingly.
References
Barrios, J M, E Benmelech, Y V Hochberg, P Sapienza, and L Zingales (2020), “Civic capital and social distancing during the COVID-19 pandemic”, NBER Working Paper 27320.
Bryan, G, and M Morten (2019), “The aggregate productivity effects of internal migration: Evidence from Indonesia”, Journal of Political Economy 127(5): 2229–68.
Ciminelli, G, and S Garcia-Mandicó (2020a), “COVID-19 in Italy: An analysis of death registry data”, VoxEU.org, 22 April.
Ciminelli, G, and S Garcia-Mandicó (2020b), “COVID-19 in Italy: An analysis of death registry data, part II”, VoxEU.org, 19 May.
Durante, R, L Guiso and G Gulino (2020a), “Civic capital and social distancing: Evidence from Italians’ response to COVID-19”, VoxEU.org, 16 April.
Durante, R, L Guiso and G Gulino (2020b), “Asocial capital: Civic culture and social distancing during COVID-19”, CEPR Discussion Papers 14820.
Fang, H, L Wang, and Y Yang (2020), “Human mobility restrictions and the spread of the novel coronavirus (2019-nCoV) in China”, NBER Working Paper 26906.
Giuffrida, A, and L Tondo (2020), “Leaked coronavirus plan to quarantine 16m sparks chaos in Italy”, The Guardian, 8 March.
Giuliano, P, and I Rasul (2020), “Compliance with social distancing during the COVID-19 crisis”, VoxEU.org, 18 June.
Gröger, A, and Y Zylberberg (2016), “Internal labor migration as a shock coping strategy: Evidence from a typhoon”, American Economic Journal: Applied Economics 8(2): 123–53.
Hsiang, S, D Allen, S Annan-Phan, K Bell, I Bolliger, T Chong, H Druckenmiller, L Y Huang, A Hultgren, E Krasovich, P Lau, J Lee, E Rolf, J Tseng and T Wu (2020), “The effect of large-scale anti-contagion policies on the COVID-19 pandemic”, Nature 584: 262–67.
Monras, J (2018), “Economic shocks and internal migration”, CEPR Discussion Paper DP12977 (last revised May 2020).
Valsecchi, M, and R Durante (2020), “Internal migration and the spread of COVID-19”, NES Working Papers w0276.
World Health Organization (2020), “Coronavirus disease (COVID-19): Situation report – 184”, 22 July.
Endnotes
1 Own calculations based on data from the Italian Civil Protection Department.
2 We include February 2020 in the pre-pandemic period since no COVID-related death was recorded in non-outbreak areas until March 2020.
3 The list of provincial controls includes: geographic characteristics (log distance to outbreak areas, size of the province, altitude, share of seaside cities); socioeconomic characteristics (share of people with high school education or higher, share of people with university education, number of firms per capita, value added per capita, median financial wealth, median income, share of urban areas); health capacity indicators (number of intensive-care beds per 100,000 inhabitants, whether the province includes the regional capital); risk factors (share of people above 70 years old, population density, share of males, whether there is an airport); and general propensity to migrate.