This year marks the 35th anniversary of Japan’s achieving preeminent status as the world’s oldest population.1 The country now boasts one of the longest ever recorded life expectancies of 84 years and the highest elderly (ages 65+) population share worldwide at 27%.2 Its primacy in this realm is expected to continue in the coming decades, leading the way through uncharted territory as ageing trends are rapidly reshaping demographics worldwide (United Nations 2015). This impressive achievement may be a double-edged sword, however – the socioeconomic burdens tied to population ageing are setting off alarm bells among experts and policymakers. Former US Secretary of Commerce Peter Peterson has referred to population ageing as “a threat more grave and certain than those posed by chemical weapons, nuclear proliferation, or ethnic strife” (Peterson 1999) and Japan’s Prime Minister, Shinzo Abe, labelled this phenomenon his country’s “biggest challenge” to address following his 2017 re-election (Yamaguchi 2017). There is no historical precedent that parallels the levels of ageing we are projected to see in the coming decades, prompting the rest of the world to sharpen its attention on Japan for leadership in designing potential solutions.
Drivers of an ageing society
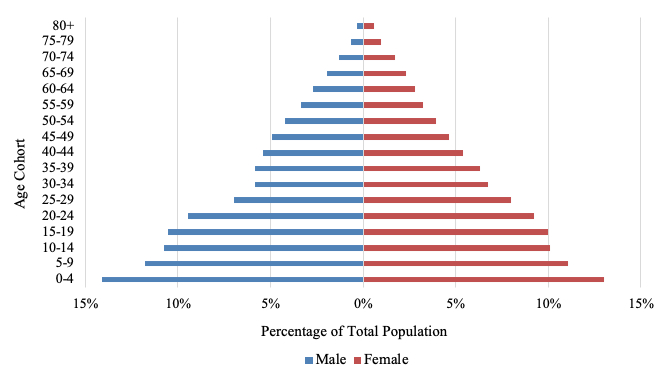
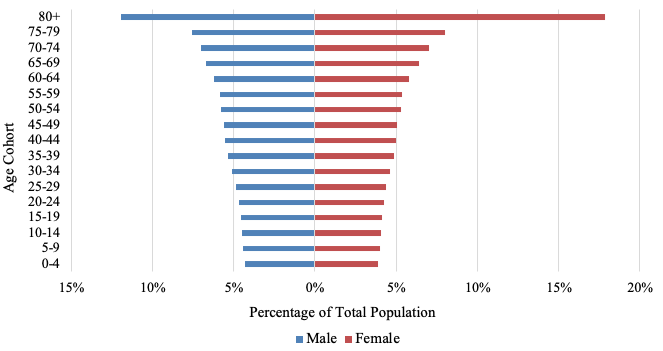
A robust combination of demographic factors is animating Japan’s age wave. The ageing of Japan’s baby boomer generation (1947–1949), which began reaching the normal retirement age of 65 in 2012, has been a large part of the impetus behind the country’s population shift. The sheer size of this cohort (8.1 million, or 6.3% of Japan’s total 2017 population) has helped dramatically reshape Japan’s population pyramid as its members have progressed to elderly ages (see Figures 1A–1C) (Japan Ministry of Health, Labour and Welfare 2008: Table 4.1, United Nations 2017). Japan’s fertility rate has also fallen steadily following the birth of this generation and is currently one of the lowest in the world at 1.5 births per woman, intensifying the age distribution’s skew away from youth (United Nations 2017). Increasing life expectancy is another driving force behind this trend. Fifty years ago, life expectancy at birth was about 72 years; it has since climbed rapidly to 84 years. Japan’s status as the country with the highest life expectancy and one of the lowest fertility rates, combined with the baby boomer generation’s progression to older ages, tells a compelling story behind its historically and comparatively unprecedented rate of population ageing.
Figure 1 Population of Japan by age and sex
a) 1950
b) 2015
c) 2050 (projected)
Source: United Nations, World Population Prospects 2017.
Note: Medium variant 2050 estimates.
Potential burdens
Rapid population ageing has become a major public policy concern in Japan. One central issue is the shrinking of the working-age population as more adults reach retirement years and fewer children are born to eventually replace them in the workforce. A dwindling workforce detracts from economic growth and impacts financial markets through reduced savings and investment levels. As discussed in one recent VoxEU column, labour force shortages in Japan can also have ‘hidden’ costs, including a decline in the overall quality of goods and services (Morikawa 2018). Exacerbating labour force shortages are the rising expenses associated with ageing, such as greater caregiving needs for the ill and infirm (which costs caretakers productive time that could be spent working on other valuable activities), and the fact that older adults are more likely to require additional medication, hospitalisation, and special services. Healthcare cost containment is an especially prominent issue for Japan, which has a relatively high share of GDP wrapped up in health spending (10.7% in 2017, the sixth-highest share among all countries).3 In addition to healthcare system obligations, an ageing society places fiscal stress on Japan through its National Pension Program as more and more adults qualify for payments. Social security payments altogether accounted for a worrisome 33.3% of Japan’s FY2017 general account government expenditures, nearly double their FY1990 share of 17.5%. These benefit payments are also growing at a faster rate than corresponding contributions, expanding the gap between insurance costs and revenues year after year and making it increasingly challenging for the government to meet its pension obligations to the eligible elderly (Japan Ministry of Finance 2017: 14).
A portfolio of solutions
Effectively addressing the public policy challenges posed by population ageing will require an integrated portfolio of complementary initiatives. Japan has already introduced a series of measures over the years that focus on these challenges. The New Angel Plan (1999) and the Plus One Policy (2009), for instance, are designed to make having children easier through initiatives such as allocating funds to new childcare facilities, reducing educational costs, and improving family housing (Centre for Public Impact 2017). Another programme under Prime Minister Abe’s comprehensive economic policy package, dubbed Abenomics, aims to increase the size of the workforce by incentivising female labour force participation. The Abenomics package also contains programmes that focus on technological innovation as a way to raise productivity (e.g. by increasing efficiency and minimising physical labour), reduce caregiver burdens (e.g. through driverless transportation or artificial intelligence), and minimise healthcare costs (e.g. through streamlined communications and remote appointment services). Other notable policy changes include programmes that invest in children’s education, which will help magnify their effective numbers at working age, and relaxing Japan’s immigration restrictions, which would augment the size of the workforce. Further, to bolster the integrity of the social security system Japan is contemplating raising the consumption tax (though this measure could admittedly be offset if it results in work disincentives or perceived intergenerational inequity).
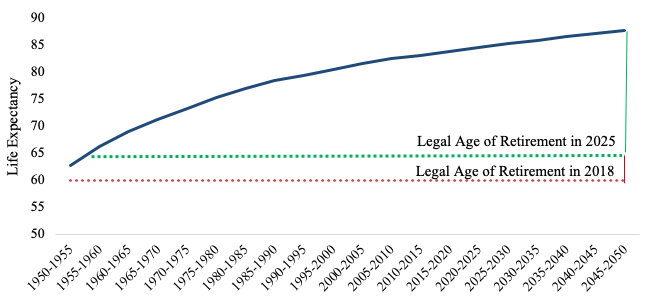
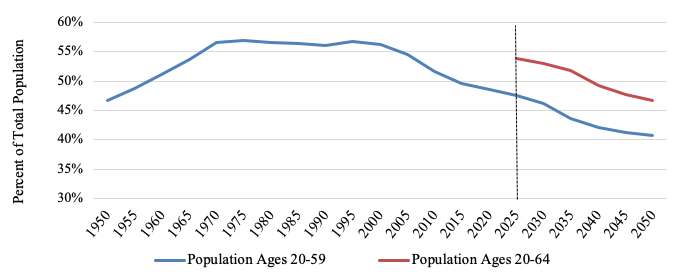
One major policy solution that Japan – among a long list of other countries, such as Austria, the UK, and Germany – has identified is raising the ages for retirement and pension eligibility. This approach may be more immediately realisable than other solutions that are not as direct, easy, or politically feasible, such as robotic automation, which may be prohibitively expensive, or raising taxes, which would be unpopular. The Japanese government is considering raising the mandatory retirement age for civil servants from age 60 to 65 and supporting private companies that retain retiree-age staff, which would help diminish the widening gap between life expectancy and the time at which individuals may exit the workforce (see Figure 2) (JapanGov 2018). This adjustment, assuming completion by 2025, would also raise the working age-to-total population ratio back to its approximate 2008 level (see Figure 3).
Japan is simultaneously adjusting the qualifying ages for pension payments – which do not depend on retirement – to reduce the fiscal pressures of population ageing. Currently, qualifying Japanese citizens may choose to start receiving pension payments from the Employees’ Pension Insurance programme at age 60 and from the National Pension Program at any point between ages 60 and 70, with the pension amount adjusted depending on the age at which payments begin.4 Japan is gradually raising the qualifying age for the Employees’ Pension Insurance programme to age 65 by 2025 for men and by 2030 for women (Clemens and Parvani 2017), and Prime Minister Abe is considering measures that would allow citizens to begin receiving National Pension Program payments after age 70 (Obe 2018). Together, these measures – raising the mandatory retirement age and the qualifying age for pension payments – would expand productive workforce years while easing the fiscal burden of pension obligations. However, and this is a critical limitation, this solution will only be viable if older adults remain healthy enough to work, to work a substantial number of hours, and to work productively as they age.
Figure 2 Japanese life expectancy estimates and projections, 1950–2050, both sexes
Source: United Nations, World Population Prospects 2017.
Figure 3 Working-age population as share of total population, Japan, 1950–2050
Source: United Nations, World Population Prospects 2017.
Note: Medium variant 2050 estimates.
Promoting elderly health
While the causal links from income to health are well established in health and development economics (Pritchett and Summers 1996), a growing line of research finds that causal links from health to income also exist (Bloom and Canning 2000). Healthier individuals are better able to continue working longer and with more energy, suggesting that protecting older individuals’ health will enhance their productivity and labour force participation (thereby magnifying the beneficial economic effects of other measures such as raising the retirement age). In addition to savings in healthcare costs, effective health promotion programmes will therefore lead to gains in productive labour hours and output. A healthier population also leads to higher savings rates, lower medical expenses, and increased foreign direct investment, all of which complement the types of policy solutions discussed above (Bloom et al. 2018, Alsan et al. 2006). These considerations reflect the fact that health interventions have socioeconomic benefits that experts and policymakers should carefully weigh as they design strategies to cope with population ageing.
Both medium- and long-term policies should feature as part of a multi-pronged approach to protecting and promoting health, including improved diets, more active lifestyles, reduced tobacco and unsafe alcohol consumption, and vaccination. Vaccination may be especially consequential among the elderly, who are particularly vulnerable to vaccine-preventable diseases such as influenza, pneumonia, and shingles (Yoshikawa 1981). Pneumonia, for instance, was the third-leading cause of death among Japan’s elderly in 2016.5 The costs of contracting infectious diseases can quickly dwarf immunisation costs for the elderly, who are more likely to require hospitalisation or to suffer from comorbid health conditions (such as hypertension and congestive heart failure) that may be exacerbated by the vaccine-preventable disease (Konomi et al. 2017, Stupka et al. 2009). This fundamental virtue of vaccination is captured by the old adage, “an ounce of prevention is worth a pound of cure”. One recent study by Konomura et al. (2017) finds that the median treatment costs for community acquired pneumonia among the elderly in Japan were $346 per outpatient episode and $4,851 per inpatient episode, whereas the cost of the 23-valent pneumococcal polysaccharide vaccine (PPV23) is less than $90 (even less with available subsidies for the elderly) (Natio et al. 2018). Although these costs are not directly comparable, they do indicate that some of the costs of vaccination may be recouped in the form of avoided medical expenses. Contracting other illnesses such as the flu can also increase susceptibility to pneumonia; a flu vaccine (advertised as costing just $32 at one Tokyo clinic)6 may therefore offer indirect preventive benefits against pneumonia. During Japan’s recent flu outbreak earlier this year, which reached record levels (Japan Times2018), a more widely accessible and efficacious flu vaccine would have helped not just to reduce the number of pneumonia cases among older adults (and likely mortality rates as well), but also to prevent hospitalization and other treatment costs, missed paid and unpaid work, and anxieties surrounding the prospect of becoming infected.
A recent poster by Sevilla et al. (2017) has shown pneumococcal vaccination to be highly effective at preventing pneumococcal disease’s socioeconomic costs among older Danish adults. The authors studied the 13-valent pneumococcal conjugate vaccine (PCV13) in Denmark and found that, among adults aged 50–85, the vaccine conservatively boasted a rate of return of almost 150%. Even more impressively, for diabetics aged 65–85, PCV13 exhibited an astounding 1,200% rate of return. These returns capture vaccination benefits in terms of averted health costs and productivity gains (market and nonmarket), demonstrating the considerable potential value of elderly vaccination through both direct and indirect avenues of benefit. While institutional differences mean the Denmark results may not be applicable to those for a similar hypothetical study in Japan, the results evidence the plausibility of such high gains and suggest that Japan’s policymakers should consider elderly vaccination as a potential source of significant benefits in light of their efforts to address the adverse effects of population ageing.
Conclusion
Population ageing will be a formidable, though not insurmountable, force to contend with in the coming decades. Japan is confronting the issues of an ageing society earlier than other countries, affording it a unique leadership opportunity to devise and implement effective responses to the socioeconomic challenges of a rapidly ageing population. The rest of the world ultimately faces the same daunting demographic shift and will be watching Japan closely for the policy adjustments, innovations, and experiments its governments and businesses make to address this phenomenon and their ensuing results. There is scope to launch a system of complementary initiatives that can lead to sustainable population growth for the future. Promoting health will naturally be a key element of such strategies.
References
Alsan M, DE Bloom and D Canning (2006), “The effect of population health on foreign direct investment inflows to low- and middle-income countries”, World Development 34(4): 613–30.
Bloom D E, M Kuhn and K Prettner (2018), "Health and economic growth", Oxford Research Encyclopedia of Economics and Finance, forthcoming.
Centre for Public Impact (2017), “Tackling the declining birth rate in Japan”, 7 April.
Clemens J and S Parvani (2017), “The age of eligibility for public retirement programs in the OECD”, Fraser Research Bulletin, Fraser Institute.
The Japan Times (2018), “Health ministry issues warning as flu epidemic rages in Japan”, 26 January.
Japan Ministry of Finance (2017), “Japanese public finance fact sheet”.
Japan Ministry of Health, Labour and Welfare (2008), “Vital Statistics of Japan”, Table 4.1
JapanGov (2018), “Abenomics: for future growth, for future generations, and for a future Japan”, September.
Konomi L, A Simaku, N Ҫomo, E Kolovani, E Ramosaҫo and E Roshi et al. (2017), “Influenza associated comorbidities”, International Journal of Science and Research 6(4): 1739–40.
Konomura K, H Nagai and M Akazawa (2017), “Economic burden of community-acquired pneumonia among elderly patients: a Japanese perspective”, Pneumonia 9: 19. https://pneumonia.biomedcentral.com/track/pdf/10.1186/s41479-017-0042-1.
Morikawa, M (2018), “Hidden inflation: Japan’s labour shortage and the erosion of the quality of services”, VoxEU.org, 31 March 31.
Natio T, H Yokokawa and A Watanabe (2018), “Impact of the national routine vaccination program on 23-valent pneumococcal polysaccharide vaccine vaccination rates in elderly persons in Japan”, Journal of Infection and Chemotherapy 24(6): 496–8.
Obe, M (2018), “Abe ready to tackle Japan’s retirement age and pension crunch”, Nikkei Asian Review, 4 September.
Peterson, P G (1999), “Gray dawn: the global aging crisis”, Foreign Affairs 78(1): 42–55.
Pritchett L and L H Summers (1996), “Wealthier is healthier”, Journal of Human Resources 31(4): 841–68.
Sevilla J P, A Stawasz, D Burnes, P B Poulsen, R Sato and D E Bloom (2017), “Calculating the indirect costs of adult pneumococcal disease and the rate of return to the 13-valent pneumococcal vaccine (PCV13) in older adults, with an application to Denmark”, Value in Health 20: A787.
Stupka J E, E M Mortensen, A Anzueto and M I Restrepo (2009), “Community-acquired pneumonia in elderly patients”, Aging Health 5(6): 763–74.
United Nations (2015), World Population Ageing, Department of Economic and Social Affairs, Population Division.
Yamaguchi, M (2017), “After election win, Abe prioritizes North Korea, aging Japan”, The Chicago Tribune, 23 October.
Yoshikawa, T T (1981), “Important infections in elderly persons”, Western Journal of Medicine 135(6): 441–5.
Endnotes
[1] Japan had the highest life expectancy among all reporting countries each year between 1983–2016, with the following exceptions: 1984 (Iceland), 2008 (Liechtenstein), 2011 (Switzerland), and 2012 (San Marino) (source: World Bank World Development Indicators 2017).
[2]Source: World Bank World Development Indicators (2017 estimates).
[3]Source: OECD; see https://data.oecd.org/healthres/health-spending.htm
[4]See http://www.nenkin.go.jp/international/english/nationalpension/nationalpension.html
[5] Source: E-stat, Vital statistics of Japan: general mortality 2016, Table 15: trends in deaths and death rates (per 100,000 population) by sex, age and cause of death.
[6]See http://pctclinic.com/influenza-vaccination. Currency conversion calculated September 2018.