There has been a great deal of recent research and publicity about increasing inequality in mortality. According to the common narrative, not only do the rich live longer than the poor, but the gap is getting bigger over time. These diverging trends have been documented for mortality at middle and older ages (e.g. Chetty et al. 2016, NAS 2015, Bosworth and Burke 2014, Pijoan-Mas and Rios-Rull 2014, Waldron 2013, Wilmoth et al. 2011), but most of the existing literature ignores developments for infants, children, and young adults. Some studies have analysed trends in overall life expectancy at birth, but this measure masks trends at younger ages, since it collapses mortality rates across all ages into a single number (e.g. Olshansky et al. 2011, Wang et al. 2013). In short, little is known about how mortality trends at younger ages have developed among advantaged and disadvantaged groups over the past decades.
In two new recent papers, we analyse mortality trends across all age groups, based on groups of poor and rich counties that we follow over time (Currie and Schwandt 2016a, 2016b). We rank all counties by their poverty rates and form groups that represent 5% shares of the overall US population. We adjust these groups over time, such that the population shares stay constant and potential changes in counties’ poverty rankings are accounted for. For these county groups we then construct age-specific three-year mortality rates for 1990, 2000, and 2010, based on 100% Census population counts and the data on deaths provided by the Vital Statistics. In total, our results are based on 21,175,011 deaths.
We find strong improvements in mortality rates for infants, children and young adults, that are strongest in the poorest counties of the US. This pattern implies that inequality in mortality strongly declined among the young. For example, deaths in the first three years of life for boys in the wealthiest counties dropped by 4.2 per 1,000 births (to a rate of 5.53) between 1990 and 2010, while the the rate declined by 8.49 per 1,000 births (to 9.79) over the same period in the poorest counties. Moreover, we document striking mortality improvements for blacks at all ages, resulting in a dramatic narrowing of the racial mortality gap.
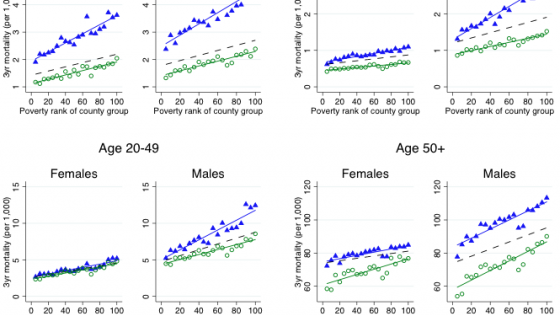
Figure 1 shows gender-specific three-year mortality rates across county groups for four broader age groups – infants and young children up to age four, children above age four and adolescents below age 20, adults of age 20 to 49, and older adults aged 50+. On each chart, there are blue triangles and green dots. The blue triangles represent death rates in 1990. The green dots represent death rates in 2010. For 2000, only a fitted line (no symbols) is shown in order to reduce clutter. Counties are grouped according to their poverty rate, so the left-most group in each chart represents the group of richest counties, while the right most group represents the poorest counties. The fitted lines are upward sloping, indicating that death rates are higher in poorer counties. A steeper slope of the regression line indicates greater inequality in life expectancy. If there was no difference in life expectancy between richer and poorer county groups, then the line would be entirely flat.
Figure 1 Three-year mortality rates across groups of counties ranked by their poverty rate

Notes: Three-year mortality rates for four different age groups are plotted across county groups ranked by their poverty rate. For further details, see the comments below Figure 2 and in the text. Mortality rates in 2000 and 2010 are age-adjusted using the 1990 population, i.e. they account for changes in the age structure within age, gender, and county groups since 1990. Table A3 provides magnitudes for individual mortality estimates and for the slopes of the fitted lines.
For the youngest age group mortality rates fall dramatically between 1990 and 2010, both for males and females, and this improvement was strongest in the poorest counties. As a result, the fitted line became much flatter, indicating a strong decrease in inequality. A similar pattern is observed for children and teens up to age 20. For adults aged 20 to 49, mortality inequality further declined for men while there is a striking stagnation for women, who did not experience any mortality improvements over the past 20 years. At older ages, mortality declined for both men and women, but these improvements were stronger in richer counties, implying increasing inequality in mortality. This is of course in line with the literature that has focused on these older age ranges.
Developments at younger ages are of particular importance because healthier children grow up to be healthier adults (Brown et al. 2015, Finch and Crimmins 2004, Miller and Wherry 2015, Wherry and Meyer 2015, Wherry et al. 2015). Our results therefore suggest that these younger cohorts will be healthier and face less inequality in mortality as they age. Moreover, mortality at young ages is a sensitive indicator of social conditions because infants and children respond more quickly to their environments. Old-age mortality, on the other hand, is largely determined by people’s past health history. Therefore, if we want to know how the health environment has changed over past decades and how the health of the future elderly will develop, looking at these younger cohorts is more informative than focusing on older ages.
Many studies have analysed mortality trends for racial subgroups, but constructing mortality rates by race is less straight-forward than one might expect. Race is recorded both in the Vital Statistics and in the Census, but the race categories don’t match across these two data sets. The Census has allowed respondents to choose multiple races since 2000, while the Vital Statistics death certificates only report one race. Since the Census population counts form the denominator of the mortality rates, using the larger multiple-race population counts will understate the mortality rate, while the rate will be overstated if only single-race counts are considered.
How relevant is multiple-race reporting? Figure 2a shows that overall rates of multi-racial reporting are still below 5% but that multiple-race reports are increasing exponentially among younger cohorts. In fact, if the current growth rate persists, the last single-race black will be born in 2050 and the last single-race white will be born in 2080 (Figure 2b). We conclude that multi-race reporting will become increasingly dominant in the future US, and that it is important to report mortality rates based both on single- and multiple-race population counts to provide upper and lower bounds for the race-specific mortality rate. Perhaps if these trends continue, the US will eventually become ‘post-racial’ after all.
Figure 2 Fraction of the black and white US population reporting multiple races
a. Census 2000 and 2010

b. Forecast

Notes: Panel a plots the fraction of people reporting multiple races among all those reporting that they are black (or white) alone or in combination, in the 2000 and 2010 Census. Panel b forecasts the fraction reporting multiple races among future birth cohorts. Assuming that the exponential growth continues, we fit a linear trend through the log fraction reporting multiple races for birth cohorts 1970 to 2010 in the 2010 Census and project this trend up to the 2080 birth cohort. The projected fraction reaches unity in 2051 for blacks and in 2081 for whites.
Figure 3a shows mortality rates at age 0-4 by county groups, separately for black and white males and females. Blue triangles show mortality rates in 1990, while green circles show rates in 2010 based on single race population counts, and red squares show the same rates based on multiple race population counts. What is most striking in these figures is the truly remarkable reduction in black mortality rates between 1990 and 2000, and the continuing, though smaller, decline for blacks between 2000 and 2010. In 1990, young black male children in the richest counties had mortality rates of 6.2 per 1000, while white male children in the poorest counties had mortality rates of about 4 per 1000. Thus, racial disparities trumped any inequality based on geographic areas. By 2010, the mortality rate for young black male children in the richest counties was still above the mortality rate for young white males in the poorest counties, but the gap had narrowed greatly. Moreover, if we use the rates calculated including people with multiple races in the denominator, the estimated black mortality rate falls even further.
Similarly striking mortality improvements for blacks can be observed at all age groups, including the middle ages for which overall mortality has been stagnating. Figure 3c shows that the stagnating mortality rates observed for females at ages 20-49 in Figure 1 are driven entirely by white females. Black females, instead, experience a 30% reduction in mortality rates in that age range.
Figure 3 Three-year white and black mortality rates across poverty percentiles, based on single and multiple race population counts
a. Age 0-4

b. Age 5-19

c. Age 20-49

d. Age 50+

Notes: 3-year mortality rates for four different age groups are plotted separately for whites and African-Americans across county groups ranked by their overall poverty rate. For further details see the comments below Figure 2 and in the text. Green circles represent mortality rates constructed as the ratio of race-specific death counts in the Vital Statistics divided by single race population counts in the 2010 Census. The mortality rates represented by red squares are based on the same death counts, but divided by population counts including multiple race reports. Mortality rates in 2000 and 2010 are age-adjusted using the 1990 population, i.e. they account for changes in the age structure within age, gender, race, and county groups since 1990.
Overall, our results show that the health of the next generation in the poorest areas of the US has improved tremendously and that the race gap has largely closed. It is surprising how little attention has been paid to this health success story in either the academic or the public discussion.
Likely drivers for the strong decline in mortality inequality are social policies that helped the most disadvantaged families. One of the most important may be expansions of public health insurance to poor pregnant women and children that took place in the late 1980s and 1990s. Other important factors include reductions in smoking prevalence, expansions of food and nutrition programs, and reductions in pollution. Overall, these findings show that even in times of great economic inequality, inequality in health outcomes is not inevitable but is strongly mediated by policy.
References
Bosworth, B P, and K Burke (2014), “Differential Mortality and Retirement Benefits in the Health and Retirement Study”, Brookings Institution Working Paper no. 2014-4.
Brown, D W, A E Kowalski, and I Z Lurie (2015), “Medicaid as an Investment in Children: What is the Long-Term Impact on Tax Receipts?”, NBER Working Paper 20835
Chetty, R, M Stepner, S Abraham, S Lin, B Scuderi, N Turner, A Bergeron, and D Cutler (2016), “The association between income and life expectancy in the United States, 2001-2014", JAMA 315 (16), 1750-1766
Currie, J, and H Schwandt (2016a), “Inequality in Mortality Between Rich and Poor U.S. Counties Decreased among the Young while Increasing for Older Adults, 1990–2010”, Science.
Currie, J, and H Schwandt (2016b), “"Mortality Inequality: The Good News from a County-Level Approach”, Journal of Economic Perspectives, 30 (2), 29-52
Finch, C E, and E M Crimmins (2004), “Inflammatory Exposure and Historical Changes in Human Life-spans”, Science 305, no. 5691, 1736-1739
Miller, S, and L R Wherry (2015), “The Long-Term Health Effects of Early Life Medicaid Coverage”, Available at SSRN
National Academy of Sciences (2015), “The Growing Gap in Life Expectancy by Income: Implications for Federal Programs and Policy Responses. Committee on the Long-Run Macroeconomic Effects of the Aging US Population-Phase II; Committee on Population, Division of Behavioral and Social Sciences and Education; Board on Mathematical Sciences and Their Applications”, Division on Engineering and Physical Sciences, Washington, DC: The National Academies Press.
Pijoan-Mas, J, and J-V Rios-Rull (2012), “Heterogeneity in Expected Longevities”, Demography 51(6), 2075-102.
Waldron, H (2013), “Mortality differentials by lifetime earnings decile: Implications for evaluations of proposed Social Security law changes”, Social Security Bulletin 73 (1)
Wherry, L R, and B D Meyer (2015), “Saving Teens: Using a Policy Discontinuity to Estimate the Effects of Medicaid Eligibility”, Journal of Human Resources, published ahead of print November 30
Wherry, L R, S Miller, R Kaestner, and B D Meyer (2015), “Child- hood Medicaid Coverage and Later Life Health Care Utilization”, NBER Working Paper 20929
Wilmoth, J R, C Boe, and M Barbieri (2011), “Geographic Differences in Life Expectancy at Age 50 in the United States Compared with Other High-Income Countries”, in E M Crimmins, S H Preston, and B Cohen (eds.), International Differences in Mortality at Older Ages: Dimensions and Sources, 337–72. Washington, DC: National Academies Press