Parental age at childbearing has increased across the Western world over the last decades, partly in response to medical advances and partly because people increasingly prefer to postpone starting a family. This development has been met with concern from medical specialists and public policymakers, as increased parental age is a potential risk factor for adverse offspring outcomes. These include stillbirth (Alio et al. 2012), low birth weight (Reichman and Teitler 2006, Schimmel et al. 2015), birth defects (Lian et al. 1986, Kazaura et al. 2004, Yang et al. 2006), pre-term birth (Zhu et al., 2005a; Fuchs et al., 2018), suicide risk (Bjørngaard et al., 2012), schizophrenia (D’Onofrio et al., 2014), and autism (Sandin et al., 2016).
Our study focuses on the relationship between parental age and birth disorders (such as clubfoot, cleft palate/lip, and birth defects of various body parts), using the population of births in Norway over an extended period (Hvide et al. 2021). The existing literature has mixed findings on the relation between parental age and offspring birth disorders, for the most part applying a cohort or case-control design where the source of age variation is parents of different age across families. The main methodological concern here is that both parental age and birth defects may correlate with difficult-to-measure or unobserved family-specific factors, such as genetic variables and factors related to socioeconomic background (Donovan and Susser 2011).
We address this methodological shortcoming by comparing outcomes of siblings. As our source of parental age variation is the same parents getting older, we hold constant many family-specific genetic and environmental factors. Using data on more than 1.2 million births from the Medical Birth Registry of Norway, we find large and convex effects of increased parental age on the increased risk of birth disorders.
Figure 1 shows that children born to parents with an average age of 45-49 were 1.9 percentage points more likely to have a birth disorders compared to children born to parents with an average age of 30–34. This is a large effect (about 70%) given that the incidence of birth disorders is 2.7% in our sample. We also find increased risk for children born to parents with an average age of 40–44. The adverse effects of parental ageing are also strong for stillbirth, low birth weight and pre-term birth.
Figure 1 The effect of parental age on likelihood of birth disorders
Notes: This figure illustrates our main results on the effect of average parental age on birth disorders, plotting the coefficients and 95% confidence intervals from an OLS regression which includes family fixed effects. Effects are relative to the reference category of average parental age being 30-34.
Data source: Norwegian Medical Birth Register, 1967–1998.
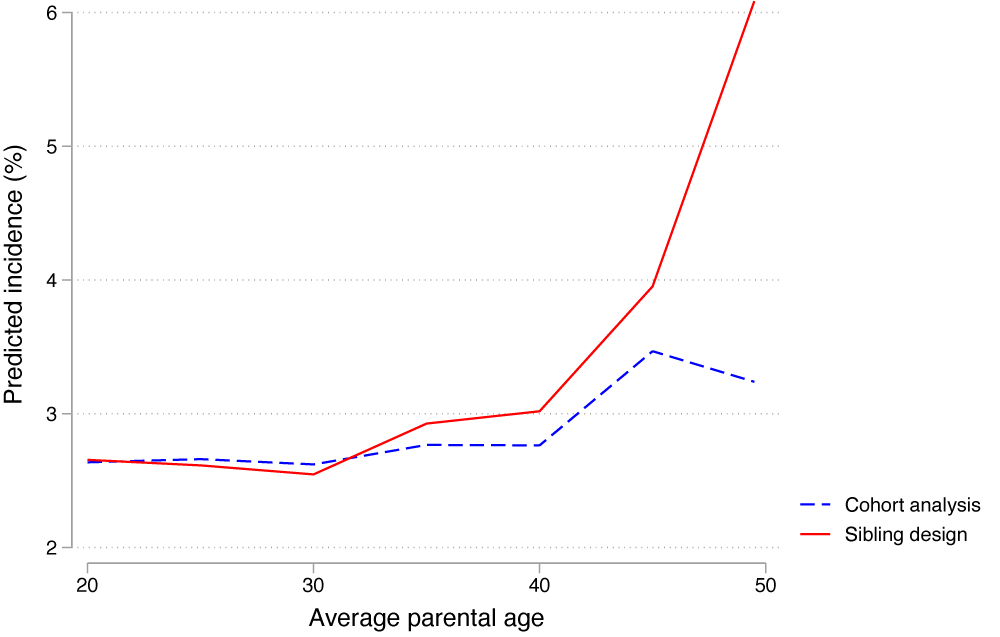
Figure 2 highlights how our study indicates that methodological shortcomings of the existing literature may have led to a large underestimation of the effects of parental aging on offspring birth defects and stillbirth. Figure 2 shows the predicted likelihood of offspring birth disorders by average parental age, comparing the results from our sibling design to the cohort analysis approach which is standard in the literature. The figure clearly illustrates that controlling for family-specific genetic and environmental factors dramatically increases the estimated risk of offspring birth disorder at older parental ages.
Figure 2 Predicted likelihood of offspring birth disorder by average parental age
Notes: This figure plots the predicted linear relationship between average parental age and the likelihood of offspring birth disorder. The y-axis indicates predicted incidence in percent. The red solid line indicates our preferred sibling design, while the blue dashed line indicates a cohort analysis.
Data source: Norwegian Medical Birth Register, 1967–1998.
The sibling design that we make use of is particularly well suited for birth outcomes, as time-varying confounders such as parental attention and sibling interaction would not have had an impact at birth. Furthermore, birth disorders are likely to originate from genetic factors so should not be impacted by in-utero related to things like household income. There are several biological mechanisms through which higher parental age can lead to higher risks of congenital anomalies – for example, paternal mutations, increased incidence of aneuploidy, and accumulation of environmental exposures over time (Eichenlab-Ritter 1996, Taylor et al. 2019, Yeshurun and Rannan 2019). There are also possible modifiers, including a healthier lifestyle with age or access to better prenatal health care.
In summary, our results indicate that the existing literature has gravely underestimated the negative effects on offspring outcomes of parental ageing. We believe our results are useful to couples that contemplate when to have children. We also believe our results are useful to policymakers and medical practitioners, when informing the general public about the potential risks of delaying having children.
References
Alio, A P, H M Salihu, C McIntosh et al. (2012), “The effect of paternal age on fetal birth outcomes”, American Journal of Men’s Health 6: 423–435.
Bjørngaard, J H, O Bjerkeset, L Vatten, I Janszky, D Gunnell and P Romundstad (2012), “Maternal age at birth, birth order, and suicide at young age: a sibling comparison”, American Journal of Epidemiology 177(7): 638–44.
D’Onofrio, B M, M E Rickert, E Frans, R Kuja-Halkola, C Almqvist, A Sjolander, H Larsson and P Lichetenstein (2014), “Paternal age at childbearing and offspring psychiatric and academic morbidity”, JAMA Psychiatry 71(4): 432–8.
Donovan, S and E Susser (2011), “Commentary: Advent of sibling design”, International Journal of Epidemiology 40: 345–349.
Eichenlaub‐Ritter, U (1996), “Parental age‐related aneuploidy in human germ cells and offspring: A story of past and present”, Environmental and molecular mutagenesis 28(3): 211-236.
Fuchs, F, B Monet, T Ducruet, N Chaillet and F Audibert (2018), “Effect of maternal age on the risk of preterm birth: A large cohort study”, PloS One 13(1): e0191002.
Hvide, H K, J Johnsen and K G Salvanes (2021), “Parental age and birth defects: a sibling study”, CEPR Discussion Paper 15836 (forthcoming in European Journal of Epidemiology).
Kazaura, M, R T Lie and R Skjærven (2004), “Paternal age and the risk of birth defects in Norway”, Annals of Epidemiology 8: 566–570.
Lian Z H, M M Zack and J D Erickson (1986), “Paternal age the occurrence of birth defects”, American Journal of Human Genetics 9: 314–319.
Reichman N E and J O Teitler (2006), “Paternal age as a risk factor for low birthweight”, American Journal of Public Health 96: 862–866.
Sandin, S, D Schendel, P Magnusson et al. (2016), “Autism risk associated with parental age and with increasing difference in age between the parents”, Molecular Psychiatry 21: 693–700.
Schimmel, M S, R Bromiker, C Hammersman, L Chertman, A Ioscovich, S Granovsky-Grisaru, A Samuleof and D Elstein (2015), “The effect of maternal age and parity on maternal and neonatal outcomes”, Archives of Gynecology and Obstetrics 291: 793–798.
Taylor, J L, J C P Debost, S U Morton et al. (2019), “Paternal-age-related de novo mutations and risk for five disorders”, Nature Communications 10(1): 1-9.
Yang, Q, S W Wen, A Leader, X K Chen, J Lipson and M Walker (2006), “Paternal age and birth defects: how strong is the association?”, Human Reproduction 22(3): 696–701.
Yeshurun, S and A J Hannan (2019), “Transgenerational epigenetic influences of paternal environmental exposures on brain function and predisposition to psychiatric disorders”, Molecular Psychiatry 24(4): 536-548.
Zhu, J L, K M Madsen, K M Vestergaard, M Basso, O and J Olsen (2005a), “Paternal age and preterm birth”, Epidemiology 16(2): 259-262.