A key contribution of health economics is to provide a framework to examine not only the direct benefits of medical innovation (such as improvements to health by taking more effective pharmaceuticals), but also the indirect effects, such as behavioural changes. For example, Papageorge (2016) shows that an important benefit of new HIV treatments emerging in the mid-1990s was to increase labour force participation. Conversely, Kaestner et al. (2014) show evidence of an increase in alcohol consumption following the introduction of statin pharmaceuticals to combat cholesterol. The key idea is that how people rethink their health-related decisions may go a long way to determining the overall effectiveness of various medical innovations.
Standard economics says that people invest in their health (Grossman 1972). Diet and exercise and wellness exams may be costly, but they are valuable in that they increase the likelihood of good health. When people experience pain, either mental or physical, people undertake costly investments to manage that pain. Consistent with this idea, when people lack good options to treat pain – perhaps due to lack of access or because existing options are stigmatised – many people may take matters into their own hands and turn to substances that are dangerous and ‘off label’ in an effort to seek relief. This behaviour, known as self-medication,1 is consistent with a long psychology literature that documents how different ailments are associated with different types of risky behaviours.
Our work connects these literatures by developing and testing a theory of rational self-medication in the context of alcohol and depression (Darden and Papageorge 2018). In our model, a stock of mental health produces depressive symptoms which can be managed contemporaneously with alcohol and/or antidepressants. At first glance, treating alcohol abuse as a costly investment in health capital may seem odd. However, the point we are making is that alcohol may be a useful way to treat the immediate symptoms of depression in the absence of better alternatives. Furthermore, the strong and persistent correlation between problem drinking and depression in US in the National Health and Nutrition Examination Survey, which we document, provides suggestive evidence that those struggling with depression may turn to alcohol. In our model, while alcohol may alleviate the immediate symptoms of depression, it may also worsen future mental health, making depressive symptoms worse in the future. The key idea behind rational self-medication is a complementarity between the symptoms of illness and the marginal utility of alcohol consumption.
To test our theory, we searched for examples in which alternative ways to manage depression improved. Rational self-medication predicts that, when safer treatment options become available, people will substitute towards them. We exploit the introduction of selective serotonin reuptake inhibitors (SSRIs), approved by the FDA in the mid-1980s to treat depression. Prior to the introduction of SSRIs, monoamine oxidase inhibitors (MAOIs) and tricyclic antidepressants (TCAs) were effective in treating depression, but severe side effects precluded widespread use. SSRIs represented a clear improvement in the choice set for managing depression and they diffused rapidly across the US. Between 2011 and 2014, roughly 13% of people aged 12 and over in the US reported using an antidepressant, and roughly 45% of those currently on an antidepressant have held their prescription for over five years (Pratt et al. 2017).
To investigate empirically, we turn to the Framingham Heart Study (FHS) Offspring Cohort, a 40-year panel of nearly 5,000 individuals in Framingham, Massachusetts. Begun in 1971 as the follow up to the FHS Original Cohort, FHS has administered repeated health and wellness exams with the goal of identifying the root causes of cardiovascular disease. The data provide rich information on alcohol consumption, antidepressant usage, and depression, in addition to the timing of other major health events and mortality. Controlling for differences across FHS participants by focusing on within-individual variation, we demonstrate prima facia evidence of substitution away from alcohol – antidepressants were associated with a 12.5% increase in alcohol abstinence following the introduction of SSRIs. These effects are stronger for men and potentially concentrated among individuals with moderate depression.
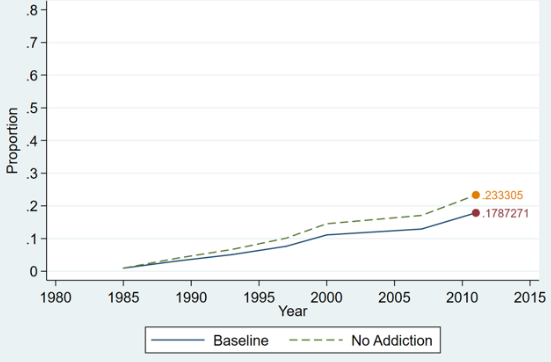
Simple regressions ignore potentially important dynamics, including addiction, which could affect how costly it is to switch from alcohol to SSRIs. Therefore, we estimate a dynamic model of alcohol and antidepressant behaviour, as well as depression and sample attrition and mortality outcomes. Figure 1 demonstrates results from simulation of this model. Figure 1a shows that when antidepressants are imposed on the sample, heavy alcohol consumption drops by 5.5 percentage points. However, this effect is driven by those with no to moderate depression – for those most heavily depressed, we simulate no change in alcohol consumption, suggesting that addiction may prevent substitution. To investigate, we simulate our model assuming that individuals did not consume alcohol in the past, removing the link between past use and the marginal utility of alcohol consumption. Figure 1b shows a significant increase in antidepressant usage overall. This effect is most significant for the most depressed. We conclude that SSRIs caused substitution away from alcohol consumption and that addiction may significantly inhibit substitution.
Figure 1a Light and heavy drinking by simulation
Note: Presents simulation results of light (Women <=7 Drinks/week; Men <=14 Drinks/week) by antidepressants.
Figure 1b Antidepressants by simulation
Note: Presents simulation results of antidepressant usage under a baseline simulation and a simulation in which past alcohol consumption is turned off, which we call the absence of addiction.
In addition to formalising the notion of self-medication, our work makes two important contributions. First, the standard economic notion of addiction is one in which, due to past use, the marginal utility of alcohol consumption is high and yet the overall level of utility is low. In this framework, it is not clear why a forward-looking person would even initiate use. Our work demonstrates a plausible reason – a rational person may begin drinking, while recognising the possibility of addiction, because alcohol alleviates pain. Indeed, Bolton (2009) show that depression and anxiety in youth (prior to any alcohol consumption) are predictive of future alcohol consumption.
Second, recent evidence from Case and Deaton (2015) documents the alarming increase in mortality rates for whites between 45-54 with a high school degree or less, the so-called deaths of despair. Our paper suggests one possible explanation for these trends. Whereas ‘despair’ technically suggests a lack of hope, self-medication suggests the opposite – heavy alcohol use or addiction may reflect an earlier, rational and hopeful attempt to medicate away pain. If so, the appropriate policy response is to stop punishing people who use risky substances to self-medicate and instead work to develop treatments that are less addictive so that people can rationally substitute away from harmful self-medicating behaviour.
The over-arching theme of our work is that policy related to innovation and research and development should consider the behavioural ramifications of new medication and therapy. Health economics, with its careful attention to the identification of causal effects in the absence of randomisation, is uniquely suited to addressing the long-term behavioural implications of technological innovations. Our work shows that, to the extent the alcohol is socially costly, the benefits of SSRIs may be understated.
References
Bolton, J M, J Robinson and J Sareen (2009), “Self-medication of Mood Disorders with Alcohol and Drugs in the National Epidemiologic Survey on Alcohol and Related Conditions”, Journal of Affective Disorders 115(3): 367-375.
Case, A and A Deaton (2015), “Rising Morbidity and Mortality in Midlife Among White Non-Hispanic Americans in the 21st Century”, Proceedings of the National Academy of Sciences 112(49): 15078-15083.
Darden, M E and N W Papageorge (2018), “Rational Self-Medication”, NBER Working Paper No. 25371.
Grossman, M (1972), “On the Concept of Health Capital and the Demand for Health”, Journal of Political Economy 80(2): 223-255.
Kaestner, R, M Darden and D Lakdawalla (2014), “Are Investments in Disease Prevention Complements? The Case of Statins and Health Behaviors”, Journal of Health Economics 36: 151-163
Papageorge, N W (2016), “Why Medical Innovation is Valuable: Health, Human Capital, and the Labor Market”, Quantitative Economics 7(3): 671-725.
Pratt L A, D J Brody and Q Gu (2017), “Antidepressant use among persons aged 12 and over: United States, 2011–2014”, National Center for Health Statistics Data Brief No. 283. Hyattsville.
Endnotes
[1] Note this is not the medical notion of self-medication, wherein one self-administers recommended or prescribed medicine.
[2] According to the online etymology dictionary, the word “despair” comes from the French-Anglo “despair”, originally the French “despoir”, referring to “hopelessness” or a “total loss of hope” (see https://www.etymonline.com/word/despair).