The impact of climate change on human health depends crucially on the adaptive strategies that humans employ to deal with rising temperatures. In an attempt to assess such strategies, ranging from increased use of air conditioning to geographic relocation, epidemiologists and economists have been examining historical evidence on the changing relationship between temperature and mortality.
Epidemiology studies such as Petkova et al. (2014), which uses data from New York City, Åström et al. (2013), using data from Sweden, as well as Hajat et al. (2002) and Carson et al. (2006), using data from London, have documented substantial changes in the relationship between temperature and mortality over the 20th century, revealing a large scope for adaptation strategies.
Economic studies such as Barreca et al. (2016) have examined how various adaptation strategies contributed to these changes. Using data from the US, mainly from the second half of the 20th century, they show that most of the changing temperature-mortality relationship can be explained by the adoption of residential air conditioning.
Examining the temperature-mortality relationship is useful as we consider the effects of a warmer future. However, research in this area is limited by the availability of high-quality historical mortality statistics. As a result, most existing studies focus on relatively wealthier locations – such as the US and Sweden – in the 20th century, when they had already achieved substantial reductions in overall mortality. Less is known about adaptation strategies that may be useful in settings with high baseline mortality rates, such as in developing countries.
In a recent paper (Hanlon et al. 2020), we introduce a new set of detailed weekly mortality data for London covering the full century 1866–1965. In this period, London’s disease environment saw enormous changes. This data set thus allows us to examine how the temperature-mortality relationship changed as the city developed.
The data also include breakdowns by cause of death, providing a window into the mechanisms through which improvements in the disease environment influenced the temperature-mortality relationship.
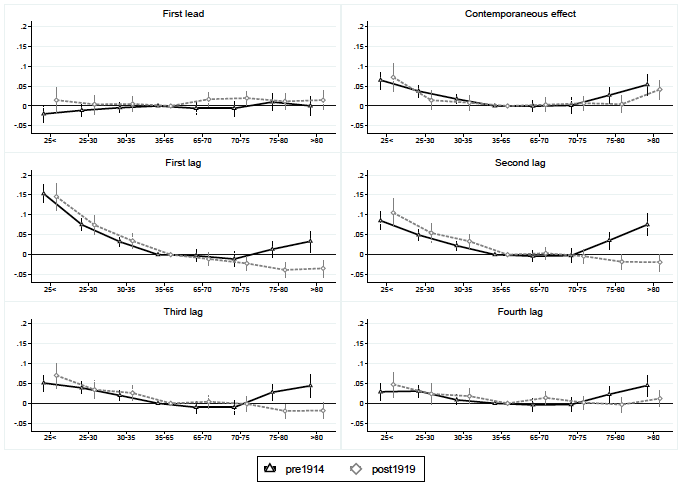
Our first main result can be viewed in Figure 1. The panels show the relationship between temperature in a particular week and mortality in: the week before (top-left panel), the week in which the temperature was measured (top-right panel), and the following four weeks (bottom four panels). Within each panel, the x-axis shows the effect of temperature falling into various bins (in Fahrenheit). The black line on the graph describes the effect before WWI, while the grey dotted line shows the effect for 1919–1965.
Figure 1 Temperature and total mortality before and after WWI
Notes: The panels show the relationship between temperature in a particular week and mortality in (1) the week before (top-left panel, ‘First lead’), (2) the week in which the temperature was measured (top-right panel, “Contemporaneous effect’), and (3) the following four weeks (bottom four panels, ‘First lag’, ‘Second lag’, ‘Third lag’, and ‘Fourth lag’). The x-axis shows the effect of temperature falling into various bins (in Fahrenheit). The black line on the graph describes the effect before WWI; the grey dotted line shows the effect for 1919–1965.
There are several striking features here. First, focusing on the top-right panel, we can see that mortality is increased by both high and low temperatures in the week in which the temperature is measured. Below that, we can see that low temperatures also increase mortality in the following four weeks and that this is true both before and after WWI.
More interesting is the impact of high temperatures. The dark line shows that high-temperature events increase mortality for several weeks for 1866–1914. However, after WWI, there is no similar increase in mortality associated with high-temperature weeks: much of the impact of high temperatures on mortality has completely disappeared.
What happened to cause such a substantial reduction in the effects of high temperatures in London in the early 20th century? The age and cause-of-death information in our new mortality series show that the high temperatures’ effect on mortality in the decades before 1914 was driven by infant deaths from digestive diseases. Around 1900, London saw a reduction in the underlying prevalence of infant digestive diseases, which then dramatically reduced the impact of high temperatures on mortality.
One implication of these findings is that changes in the underlying disease environment can substantially affect the impact of rising temperatures on human health. This suggests that improving the disease environment, particularly in the poorest locations, could be an important part of a country’s climate adaptation strategy.
Just how important could changes in the disease environment be in terms of altering the temperature-mortality relationship? We examine this question by constructing counterfactual mortality patterns. For example, suppose that the temperature-mortality relationship observed before 1914 (i.e. the black line in Figure 1) would have persisted in the decades after 1919. Our estimates show that this would have led to additional heat-related deaths equal to 0.8–1.3% of total mortality in London in the years 1919–1965.
Or, to look from another angle, we might ask what impact a 1.5-degree C increase in temperature would have had on mortality in the period before 1914 – given the temperature-mortality relationship shown in the black line – compared to the years after 1919 (grey dotted line above). Our estimates imply that a 1.5-degree increase would have generated an additional 32,061 heat-related deaths in the period before 1914, but almost no additional heat-related deaths in the decades after 1919.
Interestingly, in all periods the rise in temperature would have decreased mortality in London overall, reflecting the fact that, in all the decades of our sample, cold temperatures were associated with more deaths than high temperatures.
Examining historical mortality patterns has the potential to offer valuable insights as the world confronts the prospect of rising temperatures. Historical evidence can provide an empirical basis for assessing various adaptation strategies, ranging from expanding access to air conditioning and electricity to improving the disease environment. These lessons can guide our thinking about future conditions, and may even provide useful parameters for modelling future outcomes.
However, we should not rely only on historical evidence from relatively well-off, and therefore healthier, environments, even if those are the settings where it is easiest to access data. As our recent study shows, examining the historical temperature-mortality relationship in environments with high disease burdens can also offer insights, particularly for developing countries.
References
Åström, Daniel Oudin, Bertil Forsberg, Sören Edvinsson and Joacim Rocklöv (2013), “Acute fatal effects of short-lasting extreme temperatures in Stockholm, Sweden”, Epidemiology 24(6): 820–29.
Barreca, Alan, Karen Clay, Olivier Deschênes, Michael Greenstone and Joseph S. Shapiro (2016), “Adapting to climate change: The remarkable decline in the US temperature-mortality relationship over the 20th century”, Journal of Political Economy 124(1): 105–59.
Carson, Claire, Shakoor Hajat, Ben Armstrong and Paul Wilkinson (2006), “Declining vulnerability to temperature-related mortality in London over the 20th century”, American Journal of Epidemiology 164(1): 77–84.
Hajat, S, R S Kovats, R W Atkinson and A Haines (2002), “Impact of hot temperatures on death in London: A time series approach”, Journal of Epidemiology and Community Health 56: 367–72.
Hanlon, W Walker, Casper W Hansen and Jake Kantor (2020), “Temperature, disease, and death in London: Analyzing weekly data for the century from 1866–1965”, Journal of Economic History, forthcoming.
Petkova, Elisaveta P, Antonio Gasparrini and Patrick L Kinney (2014), “Heat and mortality in New York City since the beginning of the 20th century”, Epidemiology 25(4): 554–60.