In west Los Angeles, Century City Doctors Hospital (CCDH) is a three-mile drive from UCLA Medical Center. Recently acquired by a group of Beverly Hills doctors, CCDH has undergone $100 million in improvements in its medical care and patient amenities (CCDH, 2008). Every room is private, with a flat-screen television and organic cuisine prepared by the staff of celebrated chef Wolfgang Puck. At UCLA, by contrast, rooms are shared. But the care is world-renowned. From 2000-2004, the 30-day (risk-adjusted) mortality rate among patients with community-acquired pneumonia averaged 9.5% at UCLA, versus 9.7% at CCDH (OSHPD, 2006).
This tale of two hospitals can help us appreciate some important questions in the economics of hospital care, including:
- How do patients value hospital amenities in comparison to quality of care?
- Do the social benefits of better care and amenities at hospitals exceed the social costs?
- Are physician-owned or other hospitals relatively productive?
- Do hospitals offer better care or amenities in order to compete for patients?
The value of quality
There is substantial concern that the quality of American health care is deficient (IOM, 2001). A desire for quality improvement has prompted the development of public measures of quality of care at hospitals (DHHS, 2008). Yet the patient perspective on a hospital’s quality is likely broad enough to embody amenities in addition to quality of care (Newhouse, 1994), and appropriate measures of patients’ broad experiences with hospitals have been developed only recently (CMS, 2008).
From an economic perspective, quality is deficient only if the benefits to society of higher quality exceed the costs. Cutler and McClellan (2001) conclude that the benefits of improved treatment of heart attacks and low birthweight are roughly equal to the entire increase in U.S. medical spending from 1950 to 1990. Even so, further improvements in care may not be worthwhile (CECS, 1998). Little is known about the value of amenities to patients (Wolinksy and Kurz, 1984; Abt Associates, 2005).
The value of hospital quality also turns on its cost. Some hospitals may be able to supply high-quality care or amenities at relatively low cost. There is some evidence that the productivity of hospitals does vary. Zuckerman et al. (1992) attribute nearly fourteen percent of U.S. hospital costs to inefficiency; such inefficiency is observationally equivalent to unmeasured differences in productivity (Stigler, 1976).1 Hospitals may be more or less productive because their boards and managers are more or less effective, particularly in dealing with doctors who often enjoy substantial autonomy (Harris, 1977). An old but enduring insight in the theory of the firm is that profit-maximizing firms optimally choose their inputs and outputs based on their productivity, which is observed only imperfectly by researchers (Marschak and Andrews, 1944; Nerlove, 1965). Consistent with this insight, if relatively low-cost hospitals compete for patients by supplying high quality, a simple comparison of hospital costs and quality will understate the true cost of quality. Existing evidence on the cost of hospital care is sparse, mixed in its findings, focused on the quality of care, and unconcerned with productivity (Morey et al., 1992; Zuckerman et al., 1994; Carey and Burgess, 1999).
In recent research, we obtain insights into (if not definitive answers to) the questions posed above by appealing to patient choice behavior (Romley and Goldman, 2008). In particular, we assume that the patients we study are informed about hospital characteristics and freely choose hospitals so as to maximize their utility. The patient perspective on hospital quality is then revealed by the choices that patients make. The resulting quality measure — which we call “revealed quality” — embodies all aspects of the hospital experience that patients value, potentially including amenities as well as quality of care. We assess the importance of amenities by comparing revealed quality to the quality of care at hospitals. We are then able to consider the cost of improvements in revealed quality and quality of care. In doing so, we use patient preferences within local hospital markets to assess and account for the link between hospital productivity and quality.
Patient choice and the nature of hospital quality
We analyze the choices made by 9,008 elderly Medicare fee-for-service beneficiaries with pneumonia among 129 hospitals in greater Los Angeles in 2002. In our judgment, these choices were reasonably free. The behavior of these patients was not driven by a restricted network of providers nor by a medical emergency such as a heart attack. A patient can be admitted to a hospital only by a doctor with appropriate privileges, yet many patients report that the choice of hospital is effectively theirs to make (Wolinksy and Kurz, 1984). Patients, physicians and hospitals may associate based on quality of care or amenities; indeed, hospitals refer patients to physicians with admitting privileges. The choices made by hospital patients are also reasonably informed. Larger numbers of patients tend to obtain care at hospitals with higher-quality care (Luft et al., 1990); the introduction of public quality-of-care reports has been associated with growth in market share at high-quality hospitals (Mukamel and Mushlin, 1998). In addition, hospitals market themselves to patients based on their amenities (Gray, 1986).
In our discrete-choice model, the utility that a patient obtains from a hospital depends on the hospital’s distance from home as well as its revealed quality, with a dummy variable embodying this unobserved hospital characteristic (Berry, Levinsohn and Pakes, 1995). Intuitively, a patient chooses a hospital that is far from home only because its quality is greater than that of more convenient hospitals. A minority of the patients studied receive care at the hospital closest to home. We also analyze choice based on quality of care, as measured by hospitals’ pneumonia mortality rates.
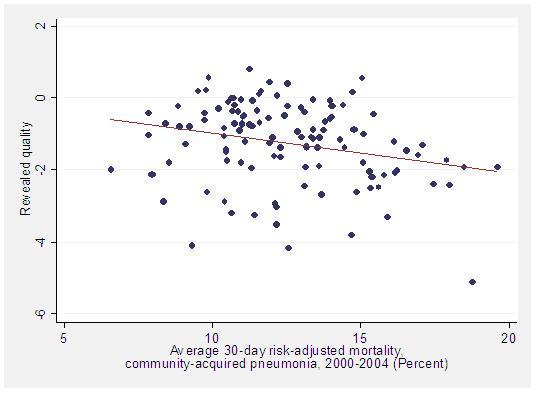
Patients do view hospitals as differentiated in revealed quality. Because revealed quality potentially embodies amenities as well as quality of care, we assess the importance of amenities by comparing revealed quality to the quality of care. Figure 1 shows that revealed quality is only modestly associated with mortality, as measured by pneumonia mortality rates. This evidence is consistent with the view that patients value, and hospitals differ in, amenities. While we have not decomposed revealed quality into its components, the results strongly suggest that some patients will sacrifice quality of care for better amenities.2
Figure 1. Revealed quality versus average pneumonia mortality rates among hospitals in greater LA
Hospital quality, costs and behavior
We are also able to analyze the cost of hospital quality.3 We first consider an inter-quartile improvement in revealed quality. We then consider an improvement in the quality of care, as measured by an inter-quartile reduction in the pneumonia mortality rate. Our hospital cost function accounts for quality, hospital scale, case mix, and inflation in factor prices.
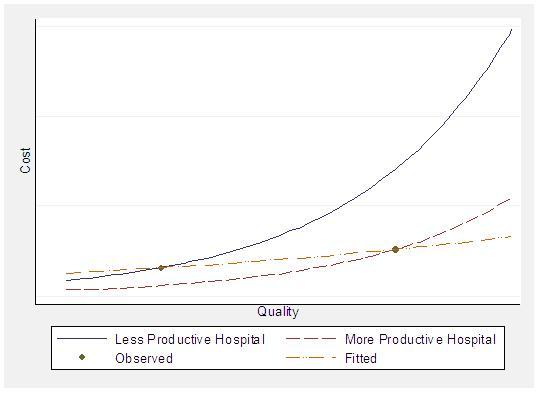
Figure 2. Regression of cost on quality understates cost of quality when more productive hospitals supply higher quality
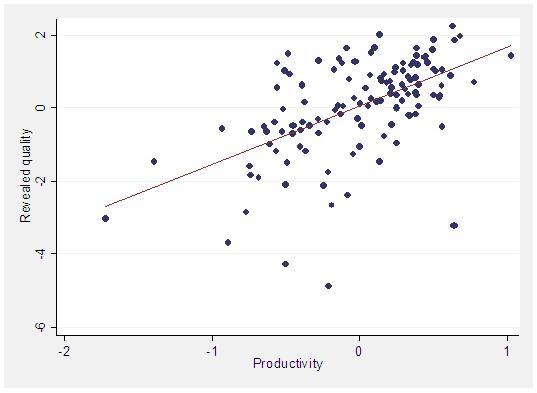
As noted earlier, a simple comparison of hospital costs and quality will understate the true cost of quality if relatively productive hospitals endogenously supply high quality. Figure 2 illustrates this situation. We deal with the problem of endogenous quality by noting that a hospital’s financial return on quality is greater when patients are more responsive to quality. Patient tastes for quality and distance did vary in our analysis of hospital choice; some patients (for example, the relatively affluent) are therefore willing to travel farther than others for a higher-quality hospital. With hospitals in greater LA competing most intensely for neighboring patients, there is variation in patient socio-demographics and tastes across localized hospital markets. We therefore use the impact of increased quality on a hospital’s demand as a source of variation in hospital quality.4 For this approach to work, this variation must be uncorrelated with unobserved productivity. This condition would be violated if, for example, patients chose where to live based on hospital productivity, which we doubt. We do find that more productive hospitals compete for patients by supplying higher revealed quality and quality of care, as Figure 3 illustrates.
Figure 3. Productivity and revealed quality among hospitals in greater LA
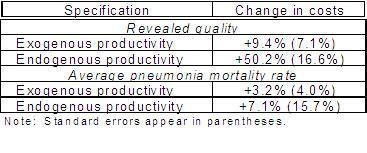
Table 1 reports our findings concerning the cost of quality. The improvement in revealed quality would increase costs by 50.2% (with a standard error of 16.6%) at the average hospital studied. Dealing with the endogeneity of productivity matters greatly for the results. When productivity is assumed to be exogenous, this quality improvement would appear to increase costs by only 9.4%. By contrast, the cost of improved quality of care is modest. With endogenous productivity, an inter-quartile reduction in the pneumonia mortality rate would increase costs by 7.1%, with a standard error of 15.7%.
Table 1. Cost of an Interquartile Improvement in Quality at Average Hospital
Implications
The evidence presented here has a variety of implications for policy and research:
- Because amenities are valued, patients can benefit from receiving worse care at a hospital with better amenities. More generally, assessments of hospital quality and performance should consider patient amenities as well as the quality of care.
- The social value of better care may exceed the social value of better amenities, given the modest cost of better care.5 The degree to which patients benefit from amenities is unknown, however, and merits study.
- The benefits of hospital quality could be modest at the margin, because health insurance mitigates financial risk by reducing the ex post price of health care. A randomized experiment has demonstrated that insurance creates some moral hazard in the consumption of medical services in hospitals (Manning et al., 1987). Medical-savings accounts and other forms of “consumer-directed health care” seek to mitigate this problem by making consumers bear more of the cost of their health care (Buntin et al., 2006). The benefits of better amenities may not be justified by their costs; nothing is known about this issue.
- Differences in hospital productivity are important. Because more productive hospitals compete for patients by supplying higher quality, a simple comparison of hospital costs and quality understates the true cost of quality. In addition, the existence of substantial productivity differences suggests that there may be meaningful opportunities for improved performance within the hospital industry. A thorough understanding of the determinants of hospital productivity might help identify such opportunities.
- With hospitals competing in quality, the resulting equilibrium may have too little or too much quality from a social perspective. A hospital’s investment in high-quality care or amenities serves to steal business from competitors, while potentially benefiting patients. Hospitals ignore the welfare of competitors or even their patients, so that private and social incentives are not aligned. Concern about a “medical arms race” has motivated certificate-of-need regulation of hospital investments in capacity and medical technologies in various U.S. states (Salkever, 2000).6 Little is currently known about competition in amenities.
References
Abt Associates (2005). Costs and Benefits of HCAHPS: Final Report. Online at http://www.cms.hhs.gov/HospitalQualityInits/downloads/HCAHPSCostsBenefits200512.pdf as of March 15, 2008.
Berry, S., J. Levinsohn and A. Pakes (1995). Automobile Prices in Market Equilibrium. Econometrica 63(4).
Buntin, M. et al. (2006). Consumer-Directed Health Care: Early Evidence about Effects on Cost and Quality. Health Affairs 25(6).
Carey, K., and J. F. Burgess, Jr. (1999). On Measuring the Hospital Cost/Quality Trade-Off. Health Economics 8(6).
Center for the Evaluative Clinical Sciences (1988). Dartmouth Atlas of Health Care 1988. Chicago, IL: American Hospital Publishing, Inc.
Centers for Medicare and Medicaid Services. The CAHPS Hospital Survey (HCAHPS). Online at http://www.hcahpsonline.org/files/Final-HCAHPS%20Fact%20Sheet_100307.pdf as of February 29, 2008.
Century City Doctors Hospital (2008). Online at http://www.ccdoctorshospital.com/site/index.htm as of March 15, 2008.
Cutler, D., and M. McClellan (2001). Is Technological Change in Medicine Worth It? Health Affairs 20(5).
Department of Health and Human Services. Hospital Compare. Online at http://www.hospitalcompare.hhs.gov/Hospital/Home2.asp?version=alternate&browser=IE%7C6%7CWinXP&language=English&defaultstatus=0&pagelist=Home as of March 15, 2008.
Gaynor, M. (2006). What Do We Know about Quality and Competition in Health Care? NBER Working Paper No. 12301.
Gray, J. (1986). The Selling of Medicine, 1986. Medical Economics 63(2).
Harris, J. (1977). The Internal Organization of Hospitals: Some Economic Implications. Bell Journal of Economics 8(2).
Institute of Medicine (2001). Crossing the Quality Chasm. Washington, DC: National Academies Press.
Luft, H.S., et al (1990). Does Quality Influence Choice of Hospital? Journal of the American Medical Association 263(21).Manning, W. et al. (1987). Health Insurance and the Demand for Medical Care: Evidence from a Randomized Experiment. American Economic Review 77(3).
Marschak, J., and W. H. Andrews, Jr. (1944). Random Simultaneous Equations and the Theory of Production. Econometrica 12(3/4).
Morey, R., et al. (1992). The Trade-Off between Hospital Quality and Cost: An Exploratory Empirical Analysis. Medical Care 30(8).
Mukamel, D., and A. Mushlin (1998). Quality of Care Makes a Difference: An Analysis of Market Share and Price Changes after Publication of the New York State Cardiac Mortality Report Cards. Medical Care 36(7).
Nerlove, M. (1965). Estimation and Identification of Cobb-Douglas Production Functions. Chicago, IL: Rand McNally.
Newhouse, J.P. (1994). Frontier Estimation: How Useful a Tool for Health Economics?. Journal of Health Economics 13(3).
Office of Statewide Health Planning and Development (2006). Community-Acquired Pneumonia in California: Hospital Outcomes in 2002-2004. Sacramento, Ca.: Healthcare Information Division.
Romley, J., and D. Goldman (2008). How Costly Is Hospital Quality? A Revealed-Preference Approach. NBER Working Paper No. 13730.
Salkever, D. (2000). Regulation of Prices and Investment in Hospitals in the United States, in Handbook of Health Economics, Culyer, A, and J. Newhouse, eds. New York: Elsevier.
Stigler, G. J. (1976). The Xistence of X-Efficiency. American Economic Review 66(1).
Wolinsky, F., and R. Kurz (1984). How the Public Chooses and Views Hospitals. Hospital and Health Services Administration 29(6).
Zuckerman, S., J. Hadley, and L. Iezzoni (1994). Measuring Hospital Efficiency with Frontier Cost Functions. Journal of Health Economics 13(3).
Footnotes
1 This “inefficiency” is also consistent with unmeasured differences in hospital quality, particularly amenities (Newhouse, 1994).
2 We interpret revealed quality as an index of quality of care and unobserved amenities. A regression of revealed quality on quality of care will decompose this index into its components only if quality of care and amenities are uncorrelated. We are unwilling to make this assumption. The hypothesis that revealed quality embodies only quality of care can nevertheless be rejected. If this hypothesis were true, revealed quality would be identical to quality of care, the fitted line in Figure 1 would lie on the 45-degree line through the origin, and the loglikelihoods of the revealed-quality and pneumonia-mortality models would be indistinguishable.
3 Expected out-of-pocket costs not vary across hospitals for the patients studied. As a result, patient costs do not affect utility or choice, and the value of quality to patients cannot be measured.
4 The derivative of a hospital’s demand with respect to its own quality depends on its actual quality, which may be related to its unobserved productivity. We purge our instrument of this influence by evaluating the derivative at the same quality level for each hospital.
5 We have not undertaken a benefit-cost analysis of the reduction in pneumonia mortality, because the cost of this improvement in the quality of care is imprecise and indistinguishable from zero.
6 This concern is particularly acute when competition in prices is limited, as was true of U.S. hospitals until the 1980s (Gaynor, 2006).